View this report

Summary
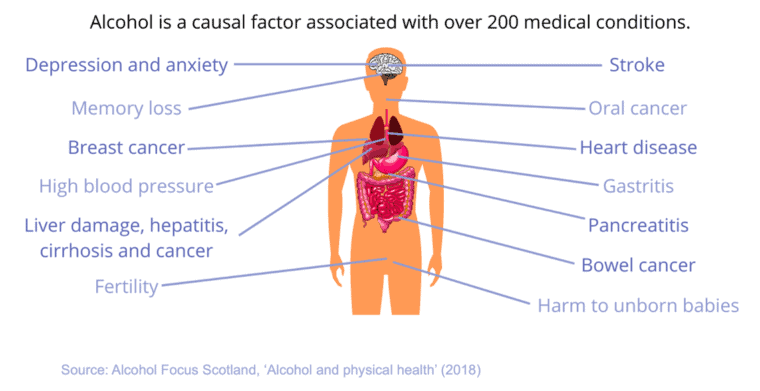
- The harmful use of alcohol is a causal factor in more than 200 disease and injury conditions
- Alcohol is metabolised in the body via oxidation and elimination
- The risks of incurring harms from drinking increase the more an individual drinks, and these harms affect the brain, the heart, the liver, digestive and endocrine systems, the immune system and many more areas of the body
- There is also convincing evidence that alcohol consumption causes cancer – it has been listed as a Group 1 carcinogen for over 30 years
Introduction
Alcohol affects health in a variety of ways; virtually every system of the human body can be damaged by its harmful consumption. The harmful use of alcohol is a causal factor in more than 200 disease and injury conditions [1].
This briefing details the ways in which alcohol affects individual physical and mental health.
The effects of alcohol on physical health
Alcohol is metabolised in the body using two processes:
- Oxidation: body cells combine oxygen with dissolved food in the bloodstream, leading to the release of heat and energy (calories) to be used for cell maintenance and repair. Alcohol calories are burnt immediately. Oxidation deals with over 90% of alcohol consumed.
- Elimination: between 2% and 10% of alcohol consumed escapes unused via breath, urine or sweat glands.
For all types of alcohol-related harm, risk increases the more an individual drinks [2]. The effects of excessive alcohol consumption are described below:
Figure 1 The effects of high-risk drinking
Brain: As a depressant of the central nervous system, alcohol interferes with the brain’s communication pathways. This occurs by the penetration of the blood-brain barrier, which otherwise prevents or slows the passage of some drugs and other harmful substances from the blood into the central nervous system. These disruptions can change mood and behaviour, and make it harder to think clearly and move with coordination. The degree to which brain activity slows down depends on how much, and how fast, a person drinks.
Some effects people experience include: altered speech; hazy thinking; slowed reaction time; dulled hearing; impaired vision; weakened muscles; and foggy memory. Over a long period of time, heavy drinkers may develop various types of physical brain damage; chronic alcohol dependence is associated with extensive brain damage and cognitive deficits leading in extreme cases to conditions such as alcoholic dementia, a loss of intellectual functioning combined with amnesia. Post-mortem studies have suggested that Wernicke-Korsakoff syndrome – one such form of alcohol-related dementia associated with alcohol misuse – occurs in about 2% of the general population and 12.5% of dependent drinkers [3].
These are due in part to the toxic effects of alcohol itself, but long term alcohol misuse can also lead to vitamin deficiencies that exacerbate the damage [4]. Alcohol-induced brain damage can be partially reversible if identified and treated in time [5].
Heart: The impact of alcohol on the heart has long been debated in the scientific literature, with recent expert opinion increasingly supporting the view that the benefits for heart health of drinking alcohol are less and apply to a smaller group of the population than previously thought. This conclusion was reached in the Chief Medical Officers’ 2016 report of the UK’s alcohol consumption guidelines. Expert evidence provided for the paper showed that the only group with potential to have an overall significant reduction in risk of death in the UK is women over the age of 55 (especially if drinking around five units a week or less), but that heart disease was a significant risk factor for heavy drinking in the short-term and regular drinking in the long-term [6].
A meta-analysis of evidence from more than 50 studies that linked drinking habits and cardiovascular health for over 260,000 people found that ‘reducing the amount of alcoholic beverages consumed, even for light-to-moderate drinkers, may improve cardiovascular health, including a reduced risk of coronary heart disease’ [7]. This has since been followed by an international review of nearly 4 million respondents from 87 studies, which has shown that previous research ‘over-estimated the possible health benefits of alcohol and under-estimated its health risks’ [8].
Whether consumed as wine, beer, or spirits, the alcohol content remains the same; a glass of wine, 250ml of ordinary strength beer and a single measure of spirits are all equal in their impact on health [9]. Therefore, large quantities of alcohol – regardless of beverage type – can affect how the heart works, and in turn, the rest of the body, for if the heart isn’t pumping blood throughout the body effectively, other organs may suffer from lack of oxygen or nutrients [10].
The pattern of consumption can also have an adverse effect on the organ’s function. Heavy consumption either during a single occasion or over a long period can cause and aggravate heart conditions such as cardiomyopathy (stretching and drooping of heart muscle) and arrhythmias (irregular heart beat), and may also lead to strokes and high blood pressure.
Liver: The liver is the major detoxifying organ of the body; it is responsible for processing what we eat and drink into nutrients and energy, as well as removing harmful substances from the blood. Most of the alcohol a person drinks is eventually broken down by the liver.
As the body cannot store alcohol, it is treated as a potential poison and eliminated via the liver, which makes it particularly vulnerable to the harmful effects of alcohol. Hence, alcoholic liver disease is the most likely type of physiological condition to result from persistent or chronic heavy alcohol consumption. The most recent official figures found alcoholic liver disease to be responsible for the majority of alcohol-related deaths in England [11].
The alcohol that is absorbed from the stomach and small intestine enters the portal vein that leads directly to the liver. The liver then effectively removes alcohol from the body by changing it to other compounds. However, too much alcohol can fast overwhelm your liver’s capacity to metabolise, and consequently your blood alcohol level rises.
Some liver damage comes from free radicals, a group of molecules that are highly reactive. These molecules can attack the nearest stable molecule, leading to a dangerous chain reaction that can result in a disease called cirrhosis of the liver. Cirrhosis occurs when scar tissue replaces normal, healthy tissue and the liver, which needs unrestricted blood flow, doesn’t work as it should [12].
The body’s natural defences against free radicals (eg antioxidants) can be inhibited by alcohol consumption, leading to increased liver damage [13]. Heavy drinking over a period of years can damage the liver, causing inflammations such as steatosis (fatty liver) alcoholic hepatitis, and fibrosis. A number of studies support a ‘small’ causal relationship between consumption and risk of developing liver cancer [14].
Digestive and endocrine systems: Alcohol is not digested like other foods; it avoids the normal digestive process and goes straight into the bloodstream. About 20% of the alcohol consumed is absorbed in the stomach, and about 80% is absorbed in the small intestine. Alcohol increases acid in the stomach, which in heavy drinkers can lead to severe stomach pain or sores in the intestines. One way to help prevent the increase of acid is by eating while drinking, as food slows down the rate at which alcohol is absorbed by the body [15].
The action of hormone release is complex. Hormones must be released at the right time, to the right tissues in the body. Alcohol can impair both the functions of the glands that release hormones and the tissues to which they are being sent. Drinking heavily can cause a steep rise in blood sugar, to which the pancreas responds by producing insulin to lower the blood sugar. But if it rises too steeply, the resulting overproduction of insulin can actually lead to low blood sugar, a condition called hypoglycaemia. This is especially dangerous for diabetics, especially those taking certain drugs to lower their blood sugar.
Alcohol also affects the endocrine system by interfering with how the body absorbs calcium, a chemical necessary for bone strength. As a result, people who drink heavily may be at a higher risk for osteoporosis, a disease in which bone density declines. If bones aren’t strong, there is a greater possibility of fractures.
Immune system and sexual health: From having frequent colds to numbness, heavy or hazardous drinking on a single occasion slows your body’s ability to ward off infections, even up to 24 hours after getting drunk. Over time, chronic drinkers are more liable to contract diseases like pneumonia and tuberculosis than those who do not drink above the recommended guidelines.
Men or boys who drink large amounts of alcohol can experience a loss of testosterone, the hormone that regulates male sexual function and semen. As a result, they could experience erectile dysfunction and emotional changes. Some women find that they are more affected by alcohol while ovulating or when they are premenstrual. This is because it takes alcohol longer to be metabolised, leading to a higher blood alcohol concentration. Women using oral contraceptives may not become intoxicated as quickly as they would otherwise, because of the contraceptive’s ability to delay the absorption of alcohol into the bloodstream.
Heavy drinking is already known to be a possible cause of infertility, but a Danish study found that even small amounts of alcohol can affect fertility [16].
Foetal Alcohol Syndrome: Exposure to alcohol can affect pregnant women too. By crossing the placental barrier, alcohol can affect a foetus by stunting its growth or weight, creating distinctive facial stigmata, and damaging the structure of the central nervous system in development. This can result in psychological or behavioural problems at birth, and physical symptoms such as an abnormally small head, defective development of mid facial tissues, minor outer ear abnormalities, abnormally small eyes, and heart and genital defects.
Foetal Alcohol Syndrome is the most involved end of the Foetal Alcohol Syndrome Disorder spectrum, a neurodevelopmental condition with lifelong cognitive, emotional and behavioural challenges. In addition to effects on the brain, FASD is a full-body diagnosis that can include more than 400 known conditions [17].
Other common diagnoses made are: Alcohol-Related Neurodevelopmental Disorder (ARND); Alcohol-Related Birth Defects (ARBD); Neurobehavioral Disorder Associated with Prenatal Alcohol Exposure (ND-PAE) [18].
Diagnosing FASDs can be hard because there is no medical test for these conditions, but some of the signs doctors look for include: prenatal alcohol exposure (although confirmation is not required to make a diagnosis); central nervous system problems (eg small head size, problems with attention and hyperactivity, poor coordination); lower-than-average height, weight, or both; and abnormal facial features (eg smooth ridge between nose and upper lip).
Cancers: The International Agency for Research into Cancer (IARC) has classified alcohol as a Group 1 carcinogen since 1988, Group 1 being the highest risk category. This means that there is convincing evidence that alcohol causes cancer [19].
Alcohol consumption may give rise to malignant tumours via the toxic metabolite acetaldehyde, which is mutagenic and can cause cancer by damaging DNA and preventing it from being repaired [20]. Drinking alcohol greatly increases the level of acetaldehyde found in saliva [21]. A small initial study published in 2012 found higher levels of DNA damage in the mouth cells of people after drinking alcohol [22].
The 2010 IARC Monograph concluded that alcohol is causally linked (to varying degrees) to several cancers – especially that of the oral cavity, pharynx (upper throat), larynx (voice box), oesophagus, liver, breast, and colorectum – and that, in many cases, the risk of cancer increases in a dose-dependent manner (ie risk increases with the volume consumed) [23].
All types of alcoholic drinks, including wine, beer and spirits, can increase the risk of cancer. The risk is linked to the actual alcohol (ethanol) in the drink [24].
A study published in 2015 found that alcohol is responsible for around 3.3% of UK cancers, 11,984 cases per year [25].
The effects of alcohol on mental health
In the long run, the effects of alcohol on the brain can be both psychological (mental health problems) and physiological (damage to brain tissue). People who drink heavily are particularly vulnerable, and alcohol is an influential factor in a number of conditions, including anxiety and depression, psychotic disorders, and suicide. For instance, it is common for people who have a mental health problem such as anxiety, depression, or schizophrenia, to ‘self-medicate’ the distressing symptoms of their condition using alcohol [26]. In England and Wales, it is estimated that alcohol is associated with 15 – 25% of all suicides and 65% of all suicide attempts. In Scotland, 53% of people committing suicide who had contact with mental health services in the 12 months prior to death had a history of alcohol misuse [27].
Alcohol dependence also delays recovery from co-existing psychiatric conditions [28]. One answer to a parliamentary question revealed that in 2012/13, there were roughly 23,000 alcohol treatment clients receiving care from mental health services for reasons other than substance misuse in England [29]. The risk of dependence jumps dramatically for men who exceed 7/8 drinks per occasion, for women 5/6 drinks per occasion (ie binge drinking levels) [30]. Heavy steady chronic drinking at sufficiently high levels can also lead to the physiological changes that result in alcohol dependence [31].
In addition, researchers who have tried to elucidate the relationship between alcohol consumption and aggression have suggested that people with a psychiatric condition called antisocial personality disorder (ASPD) may be particularly susceptible to alcohol-related aggression. One US survey of over 20,000 people found that those who met the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders criteria for ASPD (DSM-IV) were 21 times more likely to develop alcohol abuse and dependence at some point during their lives than those who did not have ASPD [32].
- World Health Organization (September 2018) ‘Alcohol’
- Anderson P (2003), ‘The Risk of Alcohol‘, PhD Thesis, Nijmegen University; The Netherlands
- Alzheimers Society, Wernicke–Korsakoff syndrome (2023)
- Alcohol Change (March 2014), ‘All in the mind – Meeting the challenge of alcohol-related brain damage’, p. 5
- Knight RG, ‘Neurological Consequences of Alcohol Use’, Chapter 7 in International Handbook of Alcohol Dependence and Problems, pp. 129–149
- Department of Health (January 2016), ‘UK Chief Medical Officers’ Alcohol Guidelines Review: Summary of the proposed new guidelines’, pp. 3–5
- ‘New study shows drinking alcohol, even light-to-moderate amounts, provides no heart health benefit’; British Medical Journal (July 2014), ‘Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data’
- Stockwell T, et al (March 2016)., ‘Do “Moderate” Drinkers Have Reduced Mortality Risk? A Systematic Review and Meta-Analysis of Alcohol Consumption and All-Cause Mortality’, Journal of Studies on Alcohol and Drugs, 77 (2), pp. 185–198
- Anderson, ‘The Risk of Alcohol‘
- Science NetLinks, ‘Alcohol and the Human Body‘, Circulatory System
- NHS Digital, ‘Statistics on Alcohol, England 2020‘ (2020)
- Science NetLinks, ‘Digestive system’
- Kurose I, Higuchi H, Kato S, Miura S, and Ishii H, ‘Ethanol-induced oxidative stress in the liver’, Alcoholism: Clinical and Experimental Research (1996), Volume 20: Issue 1, 77A–85A
- Ringborg U, ‘Alcohol and the risk of cancer’, in Alcoholism: Clinical and Experimental Research (1998), Volume 22, 323S–328S
- Science NetLinks, ‘Digestive system’
- Jensen TK, et al., ‘Does moderate alcohol consumption affect fertility?’, British Medical Journal (August 1998), Volume 317, pp. 505–510
- National Organisation for FASD (2020), ‘What is FASD?’
- Centers for Disease Control and Prevention (May 2020), ‘Basics about FASDs’
- Cancer Research UK, ‘Alcohol and cancer: the evidence’
- Bofetta P, and Hashibe, M, ‘Alcohol and Cancer’, Lancet Oncology (February 2006), Volume 7: Issue 2, pp. 149–156
- Homann N, et al., ‘High acetaldehyde levels in saliva after ethanol consumption: Methodological aspects and pathogenetic implications’, in Carcinogenesis (September 1997), Volume 18: Issue 9, pp. 1739–1743
- Balbo S et al., ‘Kinetics of DNA adduct formation in the oral cavity after drinking alcohol’, Cancer Epidemiology Biomarkers & Prevention (April 2012), Volume 21: Issue 4, pp. 601–608
- The International Agency for Research into Cancer, ‘Consumption of Alcoholic Beverages’, in A review of human carcinogens. Part E: Personal habits and indoor combustions / IARC Working Group on the Evaluation of Carcinogenic Risks to Humans (2012), Lyon, France: IARC Press, pp. 373–501
- Blot WJ, ‘Alcohol and Cancer’, Cancer Research (April 1992), Volume 52, 2119S–2l23S
- Brown K F, Rumgay H, Dunlop C, Ryan M, Quartly F, Cox A, Deas A, Elliss-Brookes L, Gavin A, Hounsome L and Huws D, ‘The fraction of cancer attributable to modifiable risk factors in England, Wales, Scotland, Northern Ireland, and the United Kingdom in 2015‘, British journal of cancer (2018) 118(8), pp. 1130–1141.
- Mental Health Foundation (October 2010), ‘Alcohol and Mental Health’, pp. 1–2
- Shepherd J, Bellis M, Hughes K, Stewart L, et al (2005)., ‘Alcohol and Violence; Briefing Statement‘, The UK Faculty of Public Health (FPH), p. 2
- Greenfield TK, ‘Individual Risk of Alcohol-Related Disease and Problems’, Chapter 21 in Heather N, Peter TJ, Stockwell T (eds) (2001), International Handbook Alcohol Dependence and Problems, John Wiley & Sons Ltd, pp. 413–439
- House of Commons Debates (November 2013), ‘Mental Illness: Drugs and Alcoholic Drinks’, c1078W
- NIAAA (2002), ‘Alcohol consumption and problems in the general population: Findings from the 1992 National Longitudinal Alcohol Epidemiologic Survey’
- The ICAP Blue Book, ‘Module 17: Alcohol dependence and Treatment’, p. 17.3
- Moeller FG, Dougherty DM, ‘Antisocial Personality Disorder, Alcohol, and Aggression’, National Institute on Alcohol Abuse and Alcoholism (NIAAA)
View this report
