In this month’s alert
Editorial – January 2019
Welcome to the January 2019 edition of Alcohol Alert, the Institute of Alcohol Studies newsletter, covering the latest updates on UK alcohol policy matters.
This month, The NHS expands the number of Alcohol Care Teams as part of its long-term plan. Other articles include: clampdown on drinking in Westminster at odds with new Health Secretary’s stance on availability and affordability of alcohol, Northern Ireland sees annual alcohol-related deaths reach an all-time high, and YouGov survey finds a quarter of Brits deliberately downplay how much they drink.
Please click on the article titles to read them. We hope you enjoy this edition.
COVER STORY – Alcohol Care Teams part of NHS long-term plan
Medics welcome nationwide extension of existing scheme
07 January 2019 – Specialist Alcohol Care Teams (ACTs) will provide treatment to patients at the 50 hospitals with the worst levels of alcohol dependence-related admissions in the country, as part of the NHS long-term plan.
The plan aims to extend a successful scheme running in hospitals located in Bolton, Salford, Nottingham, Liverpool, London and Portsmouth, where existing ACTs have significantly reduced accident and emergency (A&E) attendances, bed days, readmissions and ambulance call-outs.
The new ACTs will be funded from their clinical commissioning groups (CCGs) and health inequalities funding supplement and will work in partnership with local authority commissioners of drug and alcohol services to improve the quality of alcohol-related care. NHS England estimates that ACTs could prevent 50,000 admissions and 250,000 bed days over the next five years.
BMA board of science chair Professor Dame Parveen Kumar welcomed the plan but argued that more needs to be done, including bringing in minimum unit pricing.
She said: ‘As well as the implementation of these services in the NHS, the government needs to introduce broader measures, such as minimum unit pricing for beer, wines, and spirits, to achieve a largescale improvement in the nation’s health.
It is welcome that the government is beginning to recognise the importance of prevention and must now ensure that these plans are deliverable, sustainable, and serve the long-term needs of the public.’
You can listen to Dame Kumar speak about the NHS long-term plan for our Alcohol Alert podcast.
Heavy drinking linked with dementia
Researchers’ review of the literature identifies non-causal associations
05 January 2019 – Reducing heavy drinking may help prevent onset dementia, new BMC research suggests.
A team of Canadian and French researchers led by Jürgen Rehm, professor at the Institute for Mental Health Policy Research, conducted a scoping review of 28 papers published between 2000 and 2017 that covered the following topics:
- The associations between the volume of alcohol consumed and the incidence of cognitive impairment/dementia, which was by far the most frequent topic of reviews;
- The associations between the volume and patterns of alcohol use and specific brain structures and functions;
- Alcohol-related and -induced dementias.
The literature suggests that alcohol use is a risk factor for dementia and cognitive decline, and although a causal link could not be established, heavy alcohol use was associated with changes in brain structures, cognitive impairments, and an increased risk of all types of dementia. Light to moderate use in middle to late adulthood was associated with a decreased risk of cognitive impairment and dementia.
The report called for more research into the links between drinking and dementia. ‘Given the lack of high-quality research on alcohol, AD (Alzheimer’s disease), and cognitive functioning/impairment, future randomised prevention and secondary prevention trials with alcohol interventions are needed’, the research authors concluded.
Even ‘non-problem’ drinking by parents tied to mental health problems in kids
Adapted from Reuters Health
08 January 2019 – Kids may be more likely to develop depression and anxiety when their parents are regular drinkers, even when neither parent drinks enough to be considered an alcoholic, a Norwegian study suggests.
Researchers studied 8,773 children from 6,696 two-parent families who participated in a health survey when the kids were 13 to 19 years old. Overall, 2,132 of the children, or about 24%, had depression or anxiety, or both.
Children were 52% more likely to have anxiety or depression when both parents regularly drank alcohol and when fathers themselves had symptoms of mental health issues than when parents didn’t drink or have any psychological problems, the study found.
The findings suggest that in some family settings, even normal levels of parental alcohol use might trigger children to develop anxiety and/or depression in adolescence and early adulthood, said lead study author Ingunn Olea Lund of the Norwegian Institute of Public Health in Oslo.
‘This is significant, as the level of alcohol consumption discussed in this study rarely appears to be problematic,’ Lund said by email.
‘While the study wasn’t a controlled experiment designed to prove whether or how parents’ drinking habits might directly impact kids’ mental health, it’s possible that parents just become less attentive to children’s needs when they drink’, Lund said.
Also, changes in parents’ behaviour when they drink might be scary or uncomfortable for children, even when parents don’t consume enough alcohol to be considered problem drinkers, Lund added.
Mental health problems and alcohol use disorder in parents have long been linked to psychological problems in children, Lund’s team notes in JAMA Pediatrics. But less clear is how parents’ alcohol use that is common but not excessive might influence their children’s mental health.
On average, mothers in the study drank on about 2.6 occasions monthly and fathers drank 3.6 times monthly. The women reported consuming almost three glasses of wine, beer or liquor in a typical two-week period, while the men reported consuming more than five glasses.
Read the full article in Reuters Health.
France’s anti-addiction plan ‘low on ambition’
ANPAA delivers stinging critique of strategy
09 January 2019 – The French Government’s national plan for mobilization against addiction 2018–2022 ‘fails to provide a clear roadmap of government policy on the prevention of addictive behaviour’, according to addiction prevention campaigners ANPAA.
In their response to the announcement, the NGO welcomed the strong focus given to prevention, consistent with the nation’s health strategy and the prevention priority plan.
However, although the list of priorities is laid out clearly, displaying a good understanding of the nation’s public health issues, the objectives are low on ambition, without funding or a timetable of concrete actions.
On the issue of reducing youth exposure to alcohol advertising, ANPAA remarked that ‘the plan could have taken a stronger decision on advertising around schools and on the regulation of internet advertising and social networks to which young people are particularly sensitive’
ANPAA also regretted the absence of several measures recommended by international health authorities and recently adopted in some countries: namely minimum unit pricing; mandatory labelling of nutritional information; and Loi Évin loopholes in sports and music events.
Similarly, the government’s plan said nothing about the taxation of pre-mixed drinks based on wine, and those that are particularly aimed at young people, as well as food products that contain alcohol.
ANPAA concluded the plan is indicative of the gap between the ambitions displayed by the government and the actions it is ready to actually implement. ‘A half-hearted result which, again, shows the influence of lobbies on the executive’.
Westminster mixing messages on alcohol
Parliament tightens drinking rules while the Health Sec sees no problem with the nation’s consumption
11 January 2019 – In a strange turn of events, the House of Commons has imposed limits on the consumption, sale and promotion of alcohol across the Westminster estate, just as Health Secretary Matt Hancock told the media it was time to stop ‘punishing’ everybody by issuing diktats to the entire nation.
The Daily Mail reports that the move to limit the easy access to relatively cheap alcohol to Members of Parliament (MPs) comes amid concern about the culture of excess at parliament, which has been linked to complaints about bullying and harassment.
A meeting of the Commons commission, chaired by John Bercow and held before Christmas, decided that ‘alcohol should only be sold in designated bars, retail outlets and restaurants, and for banqueting’, that alcohol-free areas should be ‘encouraged and expanded’, and that adverts promoting alcohol ‘should not be run’.
Signs have since been put up in outlets including the Members’ Tea Room and the Terrace canteen saying ‘alcohol is no longer available to purchase’, in order to encourage ‘responsible alcohol consumption’.
However, this is at odds with the latest pronouncements made by the Secretary of State for Health Matt Hancock, who declared war on the ‘nanny state’, arguing against minimum unit pricing and claiming that a pint was ‘perfectly healthy’, according to the Sun.
The MP for West Suffolk said: ‘5% of people drank a third of all the alcohol in the country, yet many of us like a nice pint and it’s perfectly healthy.
‘I think instead of things like minimum unit pricing that some suggest, we should target measures.’
His comments met with bemusement from public health experts. In an editorial for the British Medical Journal, Alcohol Focus Scotland Chief Executive Alison Douglas and Alcohol Health Alliance UK Chair Sir Ian Gilmore stressed that ‘while Public Health England (PHE) figures suggest that less than 5% of us drink one third of all alcohol consumed, they also show that “the combination of increasing-risk, higher risk, and extreme drinkers accounts for about 25% of the population and consumes over 75% of the total self-reported alcohol consumption.”’
The article went on to say that to actively rule minimum pricing out now ‘simply does not make sense’ for the health secretary. The authors fretted that as they had previously seen ‘the extensive efforts by sectors of the industry to delay and derail Scottish legislation’, it would be ‘worrying indeed if the health secretary is listening to the views of those vested interests above those of the health community’.
Northern Ireland: annual alcohol-related deaths at all-time high
Mortality rate highest among middle-aged drinkers
16 January 2019 – Ten-year trend figures published in Alcohol Related Deaths Registered in Northern Ireland saw the number of alcohol-related deaths in Northern Ireland increase for the fourth consecutive year to the highest on record (illustrated).
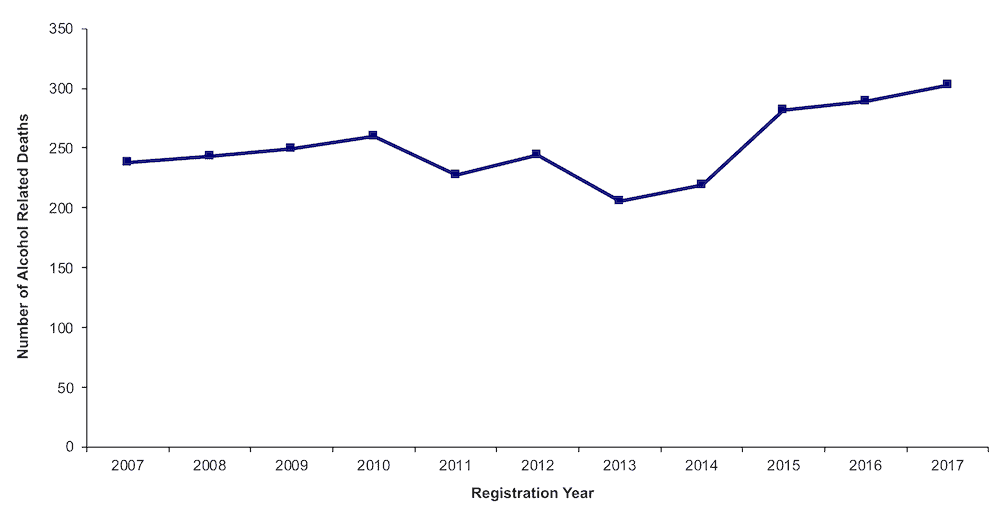
Annual number of alcohol-related deaths in Northern Ireland
|
The statistics show that 303 of the 16,036 deaths registered in Northern Ireland in 2017 (1.9%) were due to alcohol-related causes, almost 30% more than was recorded a decade previously (238) and 70% more than 2001 when the time series began (178).
Most alcohol-related deaths occurred among males, who accounted for 70% (212) of the 2017 total. The largest number of alcohol-related deaths continued to occur in those aged between 45 and 64 years. And the wealthier you were, the less likely you were to die from alcohol-related causes.
The full dataset is available at the Northern Ireland Statistics Research Agency website.
Alcohol labelling guidelines to return in September 2019?
Health minister to watch alcohol industry ‘like a hawk’
17 January 2019 – The UK Government will push for official guidelines on alcohol labelling to return in September, two years after they were quietly dropped.
Health Minister Steve Brine mentioned the fact during a House of Commons debate on foetal alcohol spectrum disorder.
He said: ‘We have been very clear with the alcohol industry that we expect the guidelines to be reflected on the labelling of all alcoholic products, and we have given the industry until September 2019 to ensure that its labelling reflects the updated guidelines.
‘The industry knows that I will be watching it like a hawk.’
In September 2017, industry body the Portman Group published a best practice guidance toolkit for drinks producers on communicating alcohol and health-related information to consumers, in consultation with the sector trade associations for drinks producers, (BBPA, NACM, SWA and WSTA), which made it optional for the chief medical officers’ guidelines to be printed on alcoholic beverages. Brine’s remark makes it more likely that this will be revised to become part of the mandatory minimum content for primary packaging.
It remains to be seen if the government is able to successfully persuade the industry to make it happen. Commenting on the move, journalist Phil Cain asked whether, even if the government does succeed, waiting for the industry was ‘the right way to regulate the sector’ in a tweet.
It is welcome news that the government is pressing for the official alcohol guidelines to return in September. But, even if it succeeds, some will look back at this episode and ask if this is the right way to regulate the sector?https://t.co/klvBvleWha
— Phil Cain (@philcaincom) 18 January 2019
Alcohol treatment common in secure settings
Alcohol most cited in new starts
17 January 2019 – Almost a third (31%) of treatment interventions in secure settings involved those who admitted to having an alcohol problem, according to the new findings from the National Drug Treatment Monitoring System (NDTMS).
55,413 adults accessed treatment in a secure setting for problematic drug use, alcohol use or both in 2017–18, of which 10,470 were for non-opiate and alcohol and 6,449 for alcohol only treatments (illustrated):
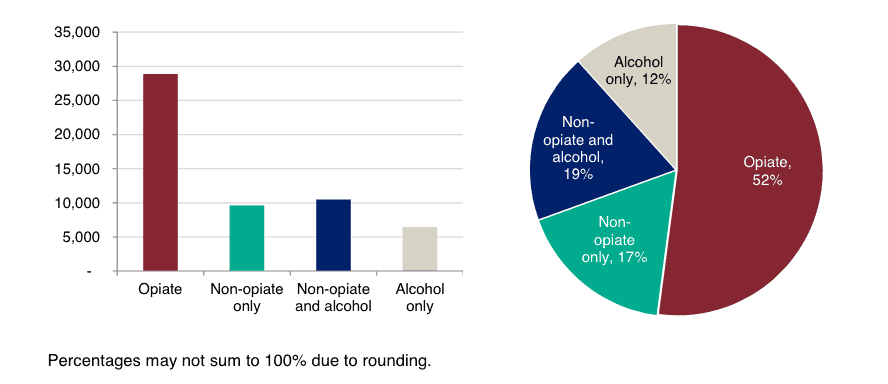
Source: Public Health England |
Overall trends show that there was a 5% fall in the number of adults in treatment in 2017–2018 compared with the previous year, the majority of which was seen within the non-opiate only (9%) and alcohol only (14%) groups.
Despite these reductions, 46% of clients starting treatment for the first time (35,689 adults) cited alcohol as problematic substance.
Adults in alcohol only treatment in secure settings tended to be older than those treated for other substances – the median age of the alcohol only group at the first point of contact with treatment was 38 years old.
Data on those with mental health issues in secure settings was collected for the first time – the proportion of people entering alcohol and drug treatment who had a mental health need other than substance misuse (which was identified and reported by healthcare services), was 32% (16,542). The proportion of people entering community alcohol and drug services who needed mental health treatment was 41% in the same period.
Calorie labelling? Let’s bottle it, say German brewers
Beer producers to phase in information this year
18 January 2019 – Beer brewers have edged ahead in the ‘race’ to determine how alcoholic beverages are labelled – the German Brewers Federation and the Private Breweries of Germany have promised to add calorie information to their bottles.
Coming almost two years after the European Commission’s challenge to alcohol producers to come up with a solution sparked a dispute between beer brewers and spirits makers, German brewers now say they will phase in new labels containing calorie information during the course of 2019.
The Straits Times reports that so far, European Union laws do not require alcoholic beverages to come with nutritional labelling. But a survey by the INSA data group for the brewers showed that 52% of German consumers would welcome such information.
The brewers say they hope winemakers and distillers will follow their example. Spirits makers, however, have long resisted adopting the beer brewers’ preferred per 100ml calorie calculation on the grounds that it is ‘inappropriate and potentially misleading in the case of spirits’, and that a per portion serving would ‘ensure that consumers can actually make realistic comparative assessments on typical calorie intake values between the different categories’.
New research centre to tackle alcohol misuse in Liverpool
TV and radio presenter Adrian Chiles among attendees
18 January 2019 – St George’s Hall in Liverpool saw the launch of a new facility looking into alcohol misuse, where TV and radio personality Adrian Chiles was on hand to speak about his own experiences with alcohol, as documented in a recent BBC programme.
The Liverpool Centre for Alcohol Research (LCAR) aims to research the reasons and consequences for the abuse of alcohol and look to develop new treatments, bringing together experts from the University of Liverpool, Liverpool John Moores University and local NHS trusts through Liverpool Health Partners.
It will focus on four main areas of research and practice and, crucially, the multidisciplinary synergies between them: liver (and other end organ) disease; mental health; cancer; and public health and associated policy.
Public health advocates are encouraged by the breadth and depth of expertise that the centre will bring to research activity into alcohol.
Alcohol Health Alliance UK Chair Professor Sir Ian Gilmore, who will be heading the LCAR, said: ‘I look forward to developing the new Liverpool Centre for Alcohol Research and to working with partners to create a leading programme of research that will have major impact on patient care at the local, national and international level.
‘Alcohol research is not a new proposition, it is the underlying strategy that is unique. Through partnership-led, translation-focused working, we hope to make advances in an area that is lacking interventions that have significant scale and reach. The increasing affordability, availability and acceptability of alcohol since the 1980s has resulted in a rising number of negative consequences that is placing a strain on the NHS, other treatment provisions, families and society in general. The recent advances made in data handling and laboratory analytics means that science is entering a new age of collaborative working that has the promise of furthering many fields. Asking the right questions and ensuring the correct skill-mix is vital to realising this potential.
‘Liverpool offers many excellent opportunities for alcohol-related research, spanning from psychology, public health and primary care, to basic science and translational research, as well as clinical studies that improve our understanding and treatment of alcohol-related conditions.’
Adrian Chiles was supportive of the new unit and recounted his recent experiences with alcohol, which featured in the BBC documentary Drinkers Like Me, originally broadcast in August 2018.
Scotland: Doctors to ask pregnant women about drink habits
Move to combat FASD part of new guidelines
23 January 2019 – Scottish experts have drawn up the first UK guidelines for diagnosing foetal alcohol spectrum disorder (FASD), in response to demands from parents for paediatricians to check their children for the condition.
Published by the Scottish Intercollegiate Guidelines Network (SIGN), which develops clinical guidelines for Scotland and is part of Healthcare Improvement Scotland, the document warns that: ‘In Scotland, many fewer children than predicted by international studies in similar populations are identified as having been affected by prenatal alcohol exposure, suggesting that we are failing to identify, and therefore adequately support, these children.’
The guidelines follow a recent study in Glasgow that studied the meconium, or stools, of newborn babies and found that 42% of samples showed evidence of the mother having consumed alcohol during pregnancy, with 15% of those pregnancies exposed to very high levels of alcohol. Only six of the 235 mothers admitted ‘light social drinking’ while pregnant.
Speaking of the guideline, Dr Patricia Jackson, Senior Fellow of Royal College of Paediatrics and Child Health, Honorary Fellow of University of Edinburgh, and Co-Chair of the Guideline Development Group, said: ‘FASD remains undiagnosed in the majority of cases. Diagnosis is currently dependent on professionals being aware of the condition and confident in carrying out a diagnostic assessment. For people with FASD, early identification and support can mean fewer mental health issues, better educational achievements, and improved life chances, reducing the possibility of later difficulties such as homelessness and involvement with the criminal justice system.
‘I would urge healthcare professionals to read the guideline and become better acquainted with how to make the diagnosis. As a result they can significantly change the lives of people with this disorder.’
Dr Catherine Calderwood, Scotland’s chief medical officer, said: ‘Early diagnosis of FASD can make a huge difference in a child’s life and these guidelines will help raise awareness of the condition among healthcare professionals.’
Alcohol makes up a fifth of catering services spending
Households data reveals how habits have changed over the last decade
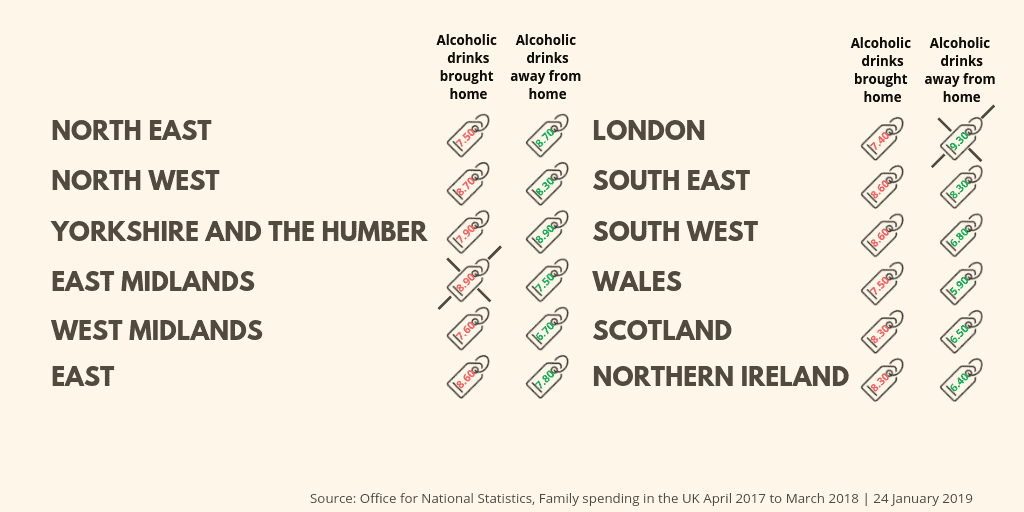
UK household expenditure on alcohol, by region |
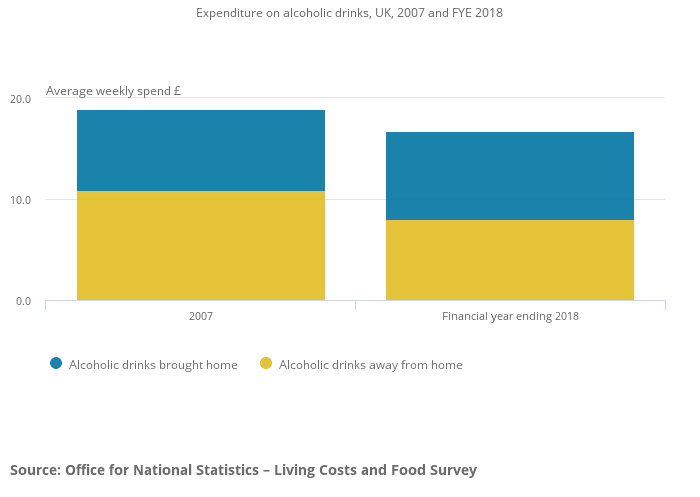
Within catering services, the second-highest spend in the financial year ending (FYE) 2018 was on alcoholic drinks away from the home, according to the new Office for National Statistics Family spending in the UK dataset.
On average, £8 per week was spent on this, accounting for 21% of household spending on catering services.
This compares with an average household spend of £8.70 on alcoholic drinks brought home, giving a total average weekly expenditure of £16.70 spent on alcoholic drinks for all households.
Combining three years of data in order to look at differences between UK countries and regions of England, the average spending on alcoholic drinks combined over financial years 2016, 2017 and 2018 was £16.00, with an average of £8.20 spent on alcoholic drinks brought home (51% of spending on alcoholic drinks) and £7.80 spent on alcoholic drinks away from home (49% of spending on alcoholic drinks).
Londoners spent the most alcoholic drinks away from home, spending an average of £9.30 a week, 56% of spending on all alcoholic drinks. The North West had the highest average weekly spend on all alcoholic drinks, at £17 per week (illustrated).
The long-term outlook for household expenditure on alcoholic drinks (including those brought home and those drunk away from the home) is one of decline. In 2007, households spent on average £18.90 on alcoholic drinks, compared with £16.70 in FYE 2018 (figures in this section have been adjusted for inflation). This is in line with a fall in the percentage of adults drinking alcohol since 2005, as reported by the Opinions and Lifestyle Survey (OPN).
 |
Quarter of Brits fib about how much they drink
GPs most likely to be lied to
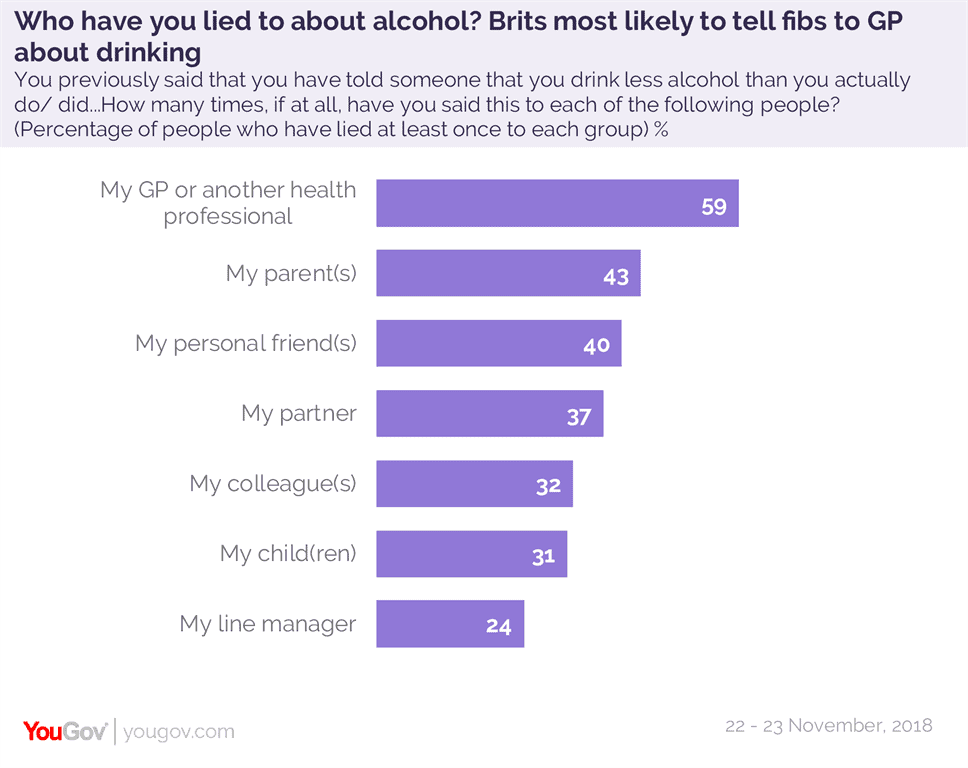 |
A new YouGov Omnibus survey confirms doctors’ suspicions about their patients’ drinking habits: just over a quarter of Brits (27%) admit they’ve told someone that they drink less alcohol than they actually do.
Of those who have deliberately downplayed the amount they consume, most have done so to their own GP – six in ten (59%, illustrated).
Four in ten (43%) have lied at least once to their parents, with one in five (21%) having lied five times or more.
Four in ten have also lied about how much they drink to their friends (40%) or partners (37%), with women almost twice as likely as men to say they have lied once to friends (10% of men vs 17% of women) or partners (9% of men vs 14% of women), and men twice as likely as women to say they have lied five times or more (15% of men vs 9% of women to a friend, 18% of men vs 8% of women to a partner).
Among those with children, a quarter (25%) of those who have previously lied about drinking habits have told their kids they drink less than they actually do. And in terms of discussing drinking at work, a third (32%) have lied to their colleagues, and a quarter (25%) have lied to a line manager.
The YouGov survey, produced for the podcast ‘Britain is a Nation Of’, interviewed 2,304 adult Brits between 22 and 23 November 2018.
ALCOHOL SNAPSHOT – As youth drinking falls, older people are drinking more
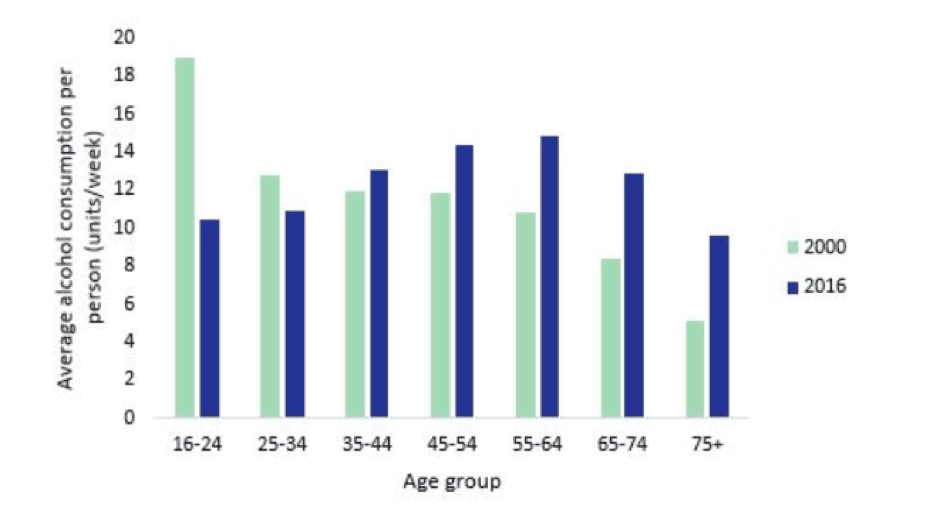
Overall alcohol consumption in the UK has fallen dramatically in recent years. Per capita alcohol sales are 15% below their 2005 peak in England, 13% below their 2007 peak in Scotland. Yet rates of harm have not declined as substantially: alcohol-related hospitalisations have increased over the period, and though alcohol-specific death rates have fallen in recent years, they remain higher than in the early 2000s.
New analysis from Colin Angus of the Sheffield Alcohol Research Group helps explain this apparent puzzle: the decline in drinking has been driven by those under 35, whereas older drinkers are in fact drinking more than in previous years. Since middle aged and older drinkers account for a greater share of deaths and hospitalisations due to alcohol, levels of consumption in this group are particularly significant in determining the level of harm.
|
The chart above, taken from a blogpost for Drink Wise Age Well, summarises Angus’ findings, which come from analysis of data from the Office for National Statistics’ General Household Survey and NHS Digital’s Health Survey for England. It shows that between 2000 and 2016, average alcohol consumption rose in every age group above the age of 35, with the largest proportionate increases in the 65-74 and 75+ age brackets. In 2000, 16-24 year olds drank by far the most alcohol. By 2016, they were among the lowest drinking groups, with only over 75s drinking less. By contrast, the heaviest drinkers are now those aged between 45 and 64.
As Angus points out, this should lead to a reconceptualisation of how we think about harmful drinking in the UK. The good news is that lower youth drinking, if sustained, should naturally reduce rates of alcohol harm in the long run. In the meantime, excessive focus on curbing the excesses of young people is a mistake, Angus suggests: ‘There is a serious danger that the good news story of falling youth drinking is distracting attention from worrying rises in levels of alcohol consumption and harm in the over 50s’. Policymakers should recognise that the best target for their policies should be the middle aged, and healthcare professionals should ensure that measures like brief interventions are focused on those in their 40s, 50s and 60s.
Podcast
Our monthly podcast features interviews with experts from across the sector.
Gambling industry harms and parallels with the alcohol world
Will Prochaska –
Coalition to End Gambling Ads

