In this month’s alert
Alcohol Duty Escalator scrapped
Government “has turned its back on public health”
David Cameron – 2012: “We can’t go on like this. We have to tackle the scourge of violence caused by binge drinking … and that means coming down hard on cheap alcohol.”
Chancellor, George Osborne, effectively read the last rites over the Government’s National Alcohol Strategy when he bowed to an intensive lobbying campaign by the alcohol industry and abolished the Alcohol Duty Escalator in his 2014 Budget. For good measure, the Chancellor also reduced the duty on beer and froze it on spirits and ordinary cider.
The Escalator, first introduced by the Labour Government in 2008, required alcohol duties to rise 2% above inflation, automatically, each year. It was seen, at the time and subsequently, as the key measure to reduce the burden of alcohol harm, and there is evidence to suggest that, over time, the Escalator was helping to reduce the number of deaths related to alcohol.
The Escalator’s abolition was greeted with delight by representatives of the alcohol industry and with dismay by the public health community.
Reacting to the announcement, Katherine Brown, Director of the Institute of Alcohol Studies, described the decision to scrap the Escalator as ‘staggering’, saying that it indicated the Government had turned its back on public health. She continued: “With alcohol costing the country £21 billion a year, and alcohol-related hospital admissions more than doubling over the last ten years, it comes as a shock to learn that the Chancellor believes that it is right to incentivize drinking further by making alcohol cheaper.”
Having also reneged on its pledge to introduce Minimum Unit Pricing of alcohol, also opposed by powerful sections of the alcohol industry, the Coalition Government is now in direct conflict with virtually the entire public health community, including, it seems, its own Department of Health. On the basis of the evidence available, the Department, like the rest of the public health community, and like the Prime Minister formerly, regards price controls as a key policy lever to tackle the health and social harm from alcohol and the huge burden it places on the public purse. At the time of going to print the Department of Health website still includes a section “Making cheap alcohol less available”, which continues:
“Too much alcohol is sold at irresponsibly low prices. Increasing the price of the cheapest drinks reduces demand from the heaviest drinkers, which in turn leads to a reduction in harm. To make it more expensive to drink excessively, we are considering introducing a minimum price per unit of alcohol. We have recently carried out a consultation to get people’s views on a minimum level of 45p per unit. We have also carried out a consultation on banning special offers (for example 2-for-1) on alcohol in shops. We will now decide on what the minimum unit price should be and whether we should ban special offers.”
There is no reference to these policies having been abandoned.
The Government has provided no justification for its rejection of price controls, despite minimum pricing of alcohol originally being presented as the central plank of its national alcohol strategy. In his Budget speech, Chancellor Osborne made only the slightest reference to the health and social costs of alcohol consumption, and no alternative policies for tackling alcohol harm, of equal effectiveness to price controls, are available. Osborne did refer to the ban on ‘below cost’ sales, but the overwhelming consensus is that this is a cosmetic measure, which will have negligible practical effect.
Prior to the Budget, the public health community had attempted to counteract the alcohol industry campaign. The Alcohol Health Alliance wrote to George Osborne urging him to stand firm and maintain the Duty Escalator. Key points mentioned in the letter included:
The alcohol duty escalator was appropriate and fair, and maintaining an upward trend in alcohol duties would be beneficial to the economy, society and public health.
The cost of alcohol harm in the UK is estimated to exceed £21bn each year, which is more than double the total revenues collected from alcohol duties (£10bn).
Reducing the affordability of alcohol is internationally recognised as one of the most effective ways of addressing alcohol harm.
Alcohol is 61% more affordable than it was in 1980, and in the UK alcohol affordability has increased significantly more than most other EU countries in recent years.
Ending the duty escalator would further weaken the ban on below cost sales.
UK wine and spirits consumption is at record levels, and among young women aged 16-24 the proportion of spirits drinkers is now larger than any other demographic group.
Professor Sir Ian Gilmore, Chair of the Alcohol Health Alliance and the Royal College of Physicians (RCP) special adviser on alcohol said:
“To suggest scrapping the duty escalator at a time when current levels of alcohol tax revenue do not even meet half the cost of alcohol related harm to our society is deplorable. Parliament has been absolutely right to support the duty escalator since 2008 – it has played an important role in addressing the affordability of cheap alcohol that creates an enormous burden on society. Government needs to stand strong on this issue – the taxpayer is already paying too much to foot the bill of alcohol related harm, now is not the time to scrap the alcohol duty escalator. Society simply cannot afford it.”
George Osborne’s complete dismissal of these considerations leaves the public health community in the position of having to accept the fact that, much rhetoric from the Prime Minister and earlier promises notwithstanding, reducing the harm from alcohol, recognised to be one of the major public health challenges of our time, is now a lost cause so long as the Coalition Government remains in power.
IAS suggests support for Minimum Pricing of alcohol greater than Government acknowledged
Having carried out an independent analysis of the results, the Institute of Alcohol Studies has concluded that the responses to the Government’s public consultation on minimum pricing (MUP) were actually more favourable to the idea than the Home Office suggested when it announced that the proposal to introduce MUP had been dropped.
The implied IAS criticism of the Government’s U-turn on minimum pricing, and of the way in which the consultation on MUP was managed and presented, is, however, mild in comparison with the vigorous denunciation published by the British Medical Journal. This claims that its investigation into the course of events discovered that “the government consultation into introducing a minimum unit price…was a sham and that politicians ignored the strong health evidence in favour of protecting the interests of industry.”
The consultation
In 2013 the Government announced it would not after all be introducing MUP, despite this previously being presented as the cornerstone of its national alcohol strategy launched a year earlier. In announcing the U-turn, Home Office Minister, Jeremy Brown, claimed that there was a lack of evidence to show that MUP would have the desired effect, and he also suggested that the consultation exercise had revealed that 56% of respondents had disagreed with the Government’s proposal to introduce a minimum price of 45p.
However, the IAS analysis of the results of the consultation shows that Mr Brown failed to distinguish between responses that were against the principle of introducing MUP at any level, and those that wanted a MUP higher than the single 45p option posed.
Additionally, the IAS also discovered that a large number of pro-MUP responses from individuals, as opposed to trade bodies, NGOs and the like, were simply excluded from the final figures as presented by the Home Office.
The main results from the IAS MUP consultation analysis report were:
Many respondents who were noted by the Home Office as against a 45p per unit minimum price were actually in favour of MUP, but at a higher minimum price of at least 50p per unit
When accounting for this discrepancy, the proportion of respondents for and against the measure was split fairly evenly (45%:46% respectively), contrary to the Home Office figures (34%:56%)
Thousands of responses from members of the public collected by Balance North East, expressing support for a 50p minimum unit price, were omitted from the published responses and Home Office calculations, whilst other submissions from individuals appear to have been accepted.
A lack of clarity about the purpose of the consultation; whether it was designed to seek views on the level or the principle of MUP and it is unclear what role the consultation responses played in the decision-making process to delay the introduction of MUP.
Katherine Brown, IAS Director said:
“Given that the consultation was designed to seek views on the level and not the principle of minimum pricing, and indeed that respondents were invited to suggest alternative levels, it is odd that the Home Office results were not presented in a way that would take this into consideration”.
“We hope that our report will provide a helpful contribution to the decision making process to introduce minimum pricing. The evidence to support this policy continues to get stronger, and this report shows there is greater public support than previously thought.”
The IAS suggests that the Government needs to use a more considered approach to gauging public opinion on proposed policies.
The full IAS report can be downloaded at:
https://www.ias.org.uk/What-we-do/IAS-reports.aspx
BMJ investigation reveals “cosy relationship” between the alcohol industry and the British government
A BMJ investigation, ‘Under the Influence’, reveals what is claimed to be the “extraordinary level of access” granted by the government to the alcohol industry “as it fought successfully last year to kill off a minimum unit pricing policy in England and Wales”.
The investigation is said to paint a vivid picture of a political class ‘both dependent on and keen to fraternise with drinks companies’ – and suggests a fundamental reluctance by the government to hamper an industry that claims credit for millions of jobs and billions of pounds of income for the Treasury.
In an open letter also published by the BMJ, senior doctors and health campaigners said that this new information “serves to fuel fears that big business is trumping public health concerns in Westminster” and they urged the government to “stop dancing to the tune of the drinks industry and prioritise the health of the public.”
The BMJ reveals that since the Coalition took power in May 2010, the Department of Health alone has had at least 130 meetings with representatives of the alcohol industry, very few of which have been publicly documented, despite a transparency initiative launched by David Cameron that same year.
These include a meeting on 12 February 2013 – six days after the close of the government’s consultation on the level at which minimum pricing should be set – between public health minister Anna Soubry and alcohol industry representatives to discuss their “deep concern” about the impending regulation.
And in April 2013 – three months after the consultation had closed and at a time when the public health community believed minimum pricing was going ahead as promised – senior executives from supermarket group Asda met with Jeremy Hunt, Secretary of State for Health, to discuss alternative measures that would not “represent a significant additional burden on our customers”.
The BMJ investigation also examined the activities of three all-party parliamentary groups that exist to support the beer, spirits and wine industries.
Current records show that the beer group, to which 300 MPs and 100 members of the House of Lords belong, received £40,000 in donations from eight companies, including Heineken, Greene King, Diageo, and Molson Coors last year.
The All-Party Scotch Whisky and Spirits Group declares no funding or other benefits received from outside sources, but its secretariat and other services are provided by the Scotch Whisky Association, which is implacably opposed to minimum pricing.
Professor Sir Ian Gilmore, special adviser on alcohol to the Royal College of Physicians and Chair of the Alcohol Health Alliance UK commented: “The drinks industry continues to have high-level access to Government ministers and officials while no forum currently exists for the public health community to put forward its case in an environment free from vested interests.”
“With deaths from liver disease rapidly rising and teenagers now presenting with advanced liver failure, the Government has a duty to realise its commitment to introduce minimum pricing.”
British Medical Journal lambasts consultation on minimum pricing as a ‘sham’
BMJ investigation reveals “cosy relationship” between the alcohol industry and the British government
A BMJ investigation, ‘Under the Influence’, reveals what is claimed to be the “extraordinary level of access” granted by the government to the alcohol industry “as it fought successfully last year to kill off a minimum unit pricing policy in England and Wales”.
The investigation is said to paint a vivid picture of a political class ‘both dependent on and keen to fraternise with drinks companies’ – and suggests a fundamental reluctance by the government to hamper an industry that claims credit for millions of jobs and billions of pounds of income for the Treasury.
In an open letter also published by the BMJ, senior doctors and health campaigners said that this new information “serves to fuel fears that big business is trumping public health concerns in Westminster” and they urged the government to “stop dancing to the tune of the drinks industry and prioritise the health of the public.”
The BMJ reveals that since the Coalition took power in May 2010, the Department of Health alone has had at least 130 meetings with representatives of the alcohol industry, very few of which have been publicly documented, despite a transparency initiative launched by David Cameron that same year.
These include a meeting on 12 February 2013 – six days after the close of the government’s consultation on the level at which minimum pricing should be set – between public health minister Anna Soubry and alcohol industry representatives to discuss their “deep concern” about the impending regulation.
And in April 2013 – three months after the consultation had closed and at a time when the public health community believed minimum pricing was going ahead as promised – senior executives from supermarket group Asda met with Jeremy Hunt, Secretary of State for Health, to discuss alternative measures that would not “represent a significant additional burden on our customers”.
The BMJ investigation also examined the activities of three all-party parliamentary groups that exist to support the beer, spirits and wine industries.
Current records show that the beer group, to which 300 MPs and 100 members of the House of Lords belong, received £40,000 in donations from eight companies, including Heineken, Greene King, Diageo, and Molson Coors last year.
The All-Party Scotch Whisky and Spirits Group declares no funding or other benefits received from outside sources, but its secretariat and other services are provided by the Scotch Whisky Association, which is implacably opposed to minimum pricing.
Professor Sir Ian Gilmore, special adviser on alcohol to the Royal College of Physicians and Chair of the Alcohol Health Alliance UK commented: “The drinks industry continues to have high-level access to Government ministers and officials while no forum currently exists for the public health community to put forward its case in an environment free from vested interests.”
“With deaths from liver disease rapidly rising and teenagers now presenting with advanced liver failure, the Government has a duty to realise its commitment to introduce minimum pricing.”
Ban on below-cost alcohol sales to come into effect before World Cup
Retailers in England and Wales will be banned from selling alcohol at ‘below-cost’ prices from April, in time for the football World Cup. Subject to Parliamentary approval, the ban will be made an additional condition of the mandatory code on alcohol retailing.
The ban will mean supermarkets and all other licensed retailers can no longer sell alcohol for less than the combined cost of government-imposed duties and value added tax (VAT).
The proposed ban on ‘below cost’ sales is the Government’s preferred alternative to the minimum unit pricing of alcohol (MUP), which the Government originally promised to introduce and which virtually the entire public health lobby favours.
According to the Home Office, the below cost ban will ‘prevent businesses from selling alcohol at heavily discounted prices and aims to reduce excessive alcohol consumption and its associated impact on alcohol related crime and health harms’.
However, health advocates lost no time in denouncing the measure as a waste of time. Prior to the Home Office announcement, analyses by the Institute of Fiscal Studies and the University of Sheffield had already indicated that a ban on below cost sales would be expected to have minimal impact on alcohol consumption, affecting less than 1% of products sold in shops and off-licences.
In contrast, a minimum unit price of 45p, as originally proposed by the Government in 2012, is predicted to have a significant impact on heavy drinkers, if introduced, preventing more than 600 alcohol-related deaths and 35,000 crimes each year.
Reacting to the Government’s announcement, Dr Keiran Moriarty, a Consultant Gastroenterologist at the Royal Bolton Hospital said:
“This is just a load of rubbish. …. A strong 440ml can of beer or lager is classed as two units, which is 25p per unit and way below the 50p minimum pricing we are calling for. This latest measure will not make any difference and does not address the real issue. They have not gone by the evidence and are trying to make it look as though they are putting something forward.”
Katherine Brown, Director of IAS said:
“Whilst we welcome the introduction of a floor price for alcohol, the ban on below cost sales sets it far too low to have any meaningful impact. Under these proposals, it will still be possible to buy two litres of strong white cider for less than £1, which is going to do nothing to curb consumption amongst children and vulnerable drinkers.
“If the Government is serious about tackling alcohol sold at pocket money prices, it must introduce minimum unit pricing. Canada has seen dramatic reductions in death rates and crimes, and all the evidence suggests that the UK would experience similar health and social benefits if the Government realised its commitment to introduce minimum pricing here.”
Earlier in the year, senior doctors and anti-alcohol misuse campaigners accused ministers of caving in to lobbying from the drinks industry over a minimum unit price.
The Government said that it had deferred introducing MUP because of a lack of evidence that it would have a sufficient impact on levels of alcohol related harm. It remains wholly unclear what evidence exists to show that the lesser measure of a ban on below cost sales is preferable.
Government failure to act on liver disease slammed by MPs
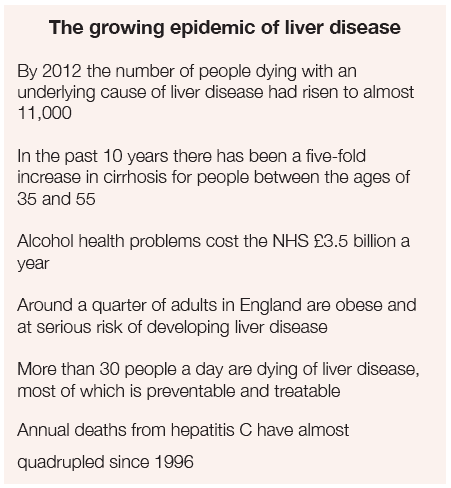
The Government’s failure to implement a strategy to combat liver disease, set to become the UK’s biggest killer within a generation, is nothing less than a scandal, according to the All-Party Parliamentary Hepatology Group of MPs in a new report. Continued failure to act, the Group says, will be catastrophic.
The Group is especially affronted by the fact that the failure to act constitutes a broken promise: despite cross-party support and support across the medical professions for a national strategy to improve outcomes in liver disease, in November 2013 plans by the Government and NHS England for a National Strategy for Liver Disease Outcomes were dropped, even though the development of a multi-stakeholder supported strategy was at its final draft stage.
It was the Government’s reneging on an earlier undertaking that prompted the All-Party Group to conduct its investigation, especially in light of the fact that deaths from liver disease have been increasing at an alarming rate in the UK, despite decreasing in most other European countries. Even more disturbing, the Group says, is the fact that the average age of death from liver disease is only 59 and continuing to fall.
Moreover, the vast majority of liver disease, caused mainly by alcohol misuse, obesity and viral hepatitis, is preventable, and yet most people at risk of developing serious liver disease, or who show early signs of liver damage, are not aware of the fact.
Yet, the Group complains, liver disease has been consistently under-prioritised and it is the only major killer lacking a national strategy.
Recommendations
The MPs’ Group makes a battery of recommendations to the Government and the Department of Health and to the NHS to produce a coherent national strategy to prevent and treat liver disease. In regard to prevention, the Group shares the disappointment of alcohol and health-related groups at the apparent abandonment of minimum unit pricing for alcohol, and the report quotes the Institute of Alcohol Studies’ comment that “the Government’s complete U-Turn on minimum pricing, which was one of the main tenets of NICE Public Health Guidance (PH24), has removed the single most effective proposed measure for combating not only alcohol misuse per se but also alcohol-related liver disease”. The Group recommends the introduction of a 50p minimum unit price for alcohol.
Report – Liver Disease: Today’s Complacency, Tomorrow’s Catastrophe: All Party Hepatology Group 2014
Harmful consequences of alcohol consumption result in over 21,000 deaths in England each year
A new report from the Centre for Public Health provides updated figures on the impact of alcohol on population health in England.Commissioned by the Department of Health, researchers at the Centre for Public Health, Liverpool John Moores University, have produced updated figures on the impact of alcohol on population health in England. These new figures will underpin future national estimates of the health impact of alcohol.
Alcohol consumption is linked to the development of many diseases and injuries. Using the latest international studies on how alcohol increases the risks of ill health and death, the report provides an update of the number of deaths and hospital admissions in 2010 that occurred as a result of alcohol consumption.
The report finds that, if only the harmful consequences are considered, over 21,000 deaths were caused by alcohol consumption, 5% of all deaths in England in 2010. This is in comparison to an estimated 6,885 deaths prevented by alcohol consumption. Alcohol-related deaths disproportionately affected younger age groups, with around 20% of all deaths in those aged under 45 years caused by alcohol.
Among under-75 year olds, years of life lost to alcohol were substantial, with over a quarter of a million potential years of life lost to alcohol-related causes. The top 3 biggest contributors were deaths from digestive diseases, injuries and cancers.
As well as contributing to deaths, alcohol places a considerable burden on health services. Using data from 2010/11, the analyses found that over 900,000 admissions to hospital were related to the harmful consequences of alcohol use, around 6% of all admission episodes in England in that year. In comparison, an estimated 101,444 hospital admissions were prevented.
Lisa Jones, Reader in Public Health from LJMU’s Centre for Public Health and lead author of the report commented: “We now know a lot more about the relationship between alcohol consumption and ill health. This data and improvements in the methodology have allowed us to identify the full impact of alcohol on population health in England”.
She continued: “These latest figures illustrate the continuing burden of alcohol to the NHS and highlight the devastating impact on our communities of the more than 21,000 deaths that occur each year from the harmful consequences of alcohol consumption.
Local Government Association calls for ‘health’ licensing objective
Local areas in England and Wales should be able to limit the opening of late-night pubs, clubs and off licences in areas where alcohol-related health problems are rife, the Local Government Association (LGA) has said.
The LGA argues that making the protection and promotion of health an objective of the licensing system would help reduce the £3.5 billion annual alcohol-related NHS bill.
In England and Wales, the Licensing Act 2003 currently has four licensing objectives: the prevention of crime and disorder, public safety, protection of children from harm, and the maintenance of public order. The Labour Government that introduced the Licensing Act deliberately excluded protection of health as a licensing objective. While the Coalition Government has amended the Act to make
Primary Care Trusts and Local Health Boards ‘responsible authorities’ under the Act and thus able to make representations in regard to licensing applications, it also decided against making protection of health a licensing objective. This is one of the LGA’s main complaints. The Association says:
“Local health experts – under the Police and Social Responsibility Act 2011 – are able to present health-related evidence, such as ambulance call-out data and hospital admissions, to councils ruling on licences. However, under government rules, councils are forced to ignore this advice when considering applications. This is restricting their ability to fulfil their public health responsibilities and protect communities.”
Cllr Katie Hall, Chair of the LGA’s Community Wellbeing Board, said:
“Councils continue to embrace their public health responsibilities to improve the health of their communities. By shifting this responsibility back to councils, the Government has rightly acknowledged they are best-placed to take local decisions for their residents.
“Local health experts have a vital role to play in advising councils on the potential impacts of an application to open new licensed premises. That makes it even more nonsensical that councils are being forced to ignore their advice when considering additional licences they know could be a health hazard.
“The Government needs to see sense and help communities by updating licensing rules and adding a new health objective. This would help improve the health of local areas and also ease the pressure on the nation’s stretched health services.”
See more at: http://www.local.gov.uk/web/guest/media-releases/-/journal_tent/56/10180/5933830/NEWS#sthash.qVFxxQb3.dpuf
Government consults on licensing fees
Trade fears ‘huge hikes’ in fees
The costs of obtaining a licence under the Licensing Act could be increased under proposals being considered by the Coalition Government, and put out for consultation.
Licensing fee levels were set in 2005 when the Licensing Act came into force in England and Wales, and they have not been changed since. Local authorities have been pressing the Government to review licensing fees, complaining that local councils are, in effect, having to subsidize the drinks industry because the current fee levels are so low that they do not even cover the costs of administering the licensing system.
The Local Government Association (LGA), which represents more than 370 councils in England and Wales, has complained that the Home Office has not made any progress on its commitment to introduce locally-set fees, set out in the 2011 Police Reform and Social Responsibility Act. This means that town halls remain unable to recover the actual costs of applications from pubs, nightclubs and off-licences. These include paying for site visits, public consultation, liaising with police, committee hearings and investigating and taking action on breaches.
It is costing councils almost £1.5 million a month with the current bill at £150 million since the system began in 2005. LGA analysis reveals this money could have:
- Provided 8.9 million hours of home care or 24.8 million Meals on Wheels
- Filled 2.8 million potholes or paid for one fifth of total council spending on street cleaning
- Funded the annual running costs of 520 libraries
- Paid for 8,430 care workers or 11,290 lollipop men and women
Cllr Mehboob Khan, Chair of the LGA’s Safer and Stronger Communities Board, said: “With council budgets on average 43% less than they were, councils are having to find £20 billion worth of savings. At a time when councils need every penny for vital services, it is totally unacceptable that councils are being forced to subsidise the drinks industry to the tune of £1.5 million a month.”
Trade Reaction
Predictably, trade bodies responded to the launch of the Government consultation by expressing concern about a possible hike in licensing fees. Brigid Simmonds of the British Beer and Pub Association warned of cash strapped local councils being tempted to increase fees dramatically, damaging local pubs. However, her statement ignored the complaint of the Local Government Association that the present level of fees is so low that local councils cannot even recoup their own costs. She also ignored the fact that the Coalition Government’s consultation is based on the premise that licensing fee levels are solely concerned with cost recovery, and that licensing fees cannot be used to raise extra revenue.
Law against alcohol sales to drunk customers ‘routinely flouted’
Bartenders readily sell more drink to those obviously incapacitated by alcohol; prosecutions rare
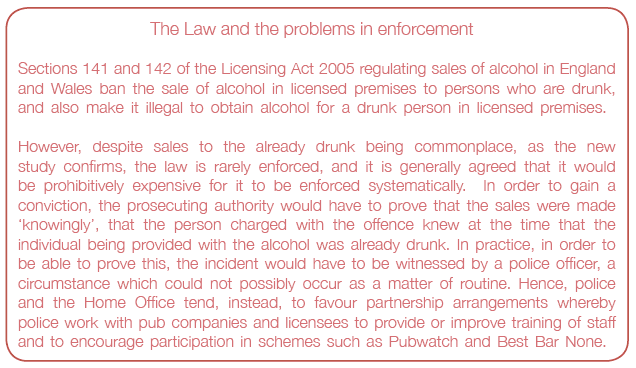
Bartenders in clubs and pubs are routinely flouting UK legislation intended to prevent further sales of alcohol to those who are already drunk, according to a study of purchase patterns in one UK city in the North West of England.
Preventing sales of alcohol to those who are already very drunk would ease the strain on public services and protect long term health, and should be a public health priority, the authors of the study say, but their research suggests that in practice such sales are commonplace. The authors base their conclusions on the results of a ‘sting’ in which student actors, aged between 20 and 22, attempted to buy alcohol while pretending to be drunk in 73 randomly selected pubs, clubs and bars in one city in North West England. All purchase attempts were made between 2100 and 0300 hours, on every day of the week bar Mondays and Tuesdays in May 2013.
One person played the fake drunk, staggering to the bar; the other took the role of the sober friend. The actors took advice from police, who regularly deal with young people who have had too much to drink on the streets of the city, to boost the authenticity of their performance.
The various venues were assessed for 10 well recognised indicators of poorly managed and problematic establishments: few seats, cheap alcohol promotions, young bartenders, young clientele, crowding, poor lighting, rowdiness, dirtiness, and prevailing levels of drunkenness.
Four out of five attempts were successful (61 out of 73, 84%), and service rates were always high, irrespective of the day or time. Sex of the purchaser made no difference to the response of the bartender.
Most sales occurred without hesitation, despite the fact that bartenders often recognised drunkenness by either commenting directly to the actor or to another server, or by rolling their eyes. And on almost one in five occasions (18%), bartenders tried to ‘upsell’ the actor a double rather than a single measure.
The likelihood of being served while drunk rose according to the number of indicators of poor management that were present. All establishments with eight or more of these indicators were prepared to serve compared with two thirds of those with none. Only greater seating provision and older bar staff boosted the odds of service refusal.
The actors were also significantly more likely to be served at venues with door supervisors (where 95% got served), but even at venues without door supervisors more than two thirds were still prepared to serve drunk individuals.
“Continued provision of alcohol to drunks will increase the risks of acute and long term health and social harms, and consequently, the burdens these place on public services and society,” comment the authors.
They go on to say that their findings suggest that the law preventing the sale of alcohol to people who are already drunk is routinely being broken, as the figures on prosecutions are low (e.g. only 3 convictions nationally in 2010).
“Although our study focused on one city, a lack of prosecution for sales to drunks throughout England suggests this is typical of nightlife environments nationally,” they say.
“With policies to prevent alcohol-related harm by increasing alcohol prices failing to be implemented, increased use of legislation preventing sales of alcohol to drunks should be considered a public health priority,” they conclude.
Does legislation to prevent alcohol sales to drunk individuals work? Measuring the propensity for night-time sales to drunks in a UK city – Online First doi 10.1136/jech-2013-203287
24-hour licensing laws fail to deliver promised cut in violence
Study finds no correlation between violent crime and flexible alcohol licensing following the 2003 Licensing Act, with researchers describing the policy intervention as ‘built on weak evidence’
A new study carried out at the University of Cambridge’s Institute of Criminology on violent crime and flexible alcohol licensing in Manchester – focusing on the two years before and two years after the introduction of the Licensing Act in late 2005 – has found no evidence that changes to licensing legislation had any effect on levels of violence.
The study authors write that the Licensing Act was a policy intervention built on ‘weak evidence that contradicted more credible and empirically supported theories about alcohol availability and harm’ and call for better communication between policymakers and researchers in the development of future preventive policies.
The new research may be seen as the final nail in the coffin of the extraordinary claims made for the 2003 Licensing Act – introduced by the Labour Government – which allowed pubs, clubs and off-licences to apply for later licensing hours beyond the traditional 11pm closing time. Apart from supposed benefits to tourism, the principal aim of the Act, and virtually its sole non-commercial objective, was stated to be a reduction in crime and disorder.
The White Paper ‘Time for Reform’ which announced the changes, insisted that one of the main problems with the then existing licensing arrangements was their actually causing public disorder ‘through standard closing hours which mean that large numbers of drinkers come out onto the streets late at night at the same time.’ It also made the suggestion, one supported enthusiastically by the alcohol trade, politicians and many in the media, that the existing ‘artificial’ closing times were an important cause of binge drinking as people tried to ‘beat the clock’.
The White Paper actually stated that ‘research indicates” that de-regulated closing times, by spreading the period during which customers leave, should produce the following key outcomes:
‘A more gradual and orderly pattern of dispersal of peak densities between the hours of 11pm-12 midnight, and 2am and 3am in urban centres
‘Significant reductions in reports of drink-related offences and in arrests for such offences
‘Reductions in binge drinking and drunkenness on the streets’
These claims are repeated in the Regulatory Impact Assessment, and the Guidance issued by the Secretary of State in regard to the operation of the Act.
However, the White Paper failed to explain that the ‘research’ on which the Government was relying, and which presumably was the source of the ‘weak evidence’ referred to by the Cambridge criminologists, was contained in a report produced for the alcohol industry, some representatives of which had been lobbying for extended drinking hours.
The new study used data from Greater Manchester Police and the Local Authority to compare recorded rates of violence with licensed trading hours in wards across the city from February 2004 to December 2007 – roughly two years either side of legislative change.
While some premises kept the previous closing time, others started to sell alcohol later into the night. Researchers investigated the extent to which licensed closing times had become staggered in neighbourhoods across Manchester after the Licensing Act was implemented.
They found that, on average, there was between 27-32% reduction in the concentration of closing times on weekdays and between 48-53% on weekends.
The researchers found no evidence to support the Labour Government’s claims that the increased staggering of closing times would result in lower rates of violence.
Researchers also investigated the claims of the Act’s critics that increases in licensed alcohol availability would lead to increased violence and disorder. When cross-referencing police records of street violence with changes to licensing hours across the city, the researchers found no evidence that increases in alcohol availability had any association with increases in levels of violence.
Part of the explanation of the absence of any discernable increase in violence is that the licensing reforms had less impact on closing times than was anticipated. Following the implementation of the Act, average trading times in Manchester only increased between 30 to 45 minutes per premise on weekdays and by 1 hour and 20 minutes at weekends – far lower than had been expected.
Commenting on the relationship between evidence and policy, or the lack of one, lead researcher, Dr David Humphreys, said:
“Over the past decade, England and Wales have witnessed a series of political prevention initiatives for alcohol-related harm that have been implemented largely without evaluation or systematic appraisal. This has resulted in missed opportunities to generate evidence, and a missed opportunity to learn, both of and from, any mistakes.”
Humphreys pointed to the recent announcement of a ‘late night levy’ in Newcastle – where premises serving beyond midnight will have to pay additional fees – as the latest in a long list of initiatives to tackle alcohol-related crime that lacks ‘any plans to rigorously investgate effectiveness’.
In the study, the authors write that opportunities to generate better evidence about the effects of the flexible licensing policy may have been missed due to the lack of government attention to monitoring and evaluation.
“While the emphasis on change and improvement should be encouraged, the enthusiasm to act needs to be balanced with careful and systematic attempts to understand the implications and effectiveness of these interventions,” Humphreys said.
The study found some evidence to suggest that areas in which the density of alcohol outlets increased might be associated with increases in violence, regardless of individual licensing – although researchers describe this evidence as ‘weak’.
– See more at: http://www.cam.ac.uk/research/news/violence-rates-unaffected-by-24-hour-licensing-laws#sthash.FT7UhL0U.dpuf
Guide to Alcohol for Councillors published by Alcohol Concern
The Guide to Alcohol for Councillors is written for councillors looking to meet the new commissioning challenges and tackle the impact of alcohol misuse in their communities. It follows the transfer of responsibility for public health from the health service to local government. The aim is to highlight all of the many areas where alcohol has an impact on a council’s local community and to demonstrate that prioritising action on alcohol misuse can have huge benefits and deliver cost savings in the long term.
Eric Appleby, Chief Executive of Alcohol Concern said:
“With local authorities taking responsibility for public health there is a huge opportunity to begin tackling alcohol harms at a local level and to save lives and cut crime.
“We know that the cost of alcohol misuse is enormous and that it takes its toll on so many aspects of our communities, whether it’s policing, providing hospital treatment or supporting children living with parents with an alcohol problem.
“We produced this guide to illustrate to councillors the extent of the damage done by alcohol misuse and to support them to develop a robust and effective alcohol strategy which benefits their entire community.”
The guide shows local councils how alcohol misuse has an impact on all of their departments and many of the services they deliver, from children and families to adult social care, from housing to treatment services for those suffering from alcohol misuse, as well as dealing with crime and antisocial behaviour, cleaning up drink related rubbish and road safety. It offers basic, practical information on alcohol, from recommended weekly units to the drink drive limits. It also includes information on where to seek further help and advice on various alcohol issues when necessary.
Jonathan McShane, Cabinet Member for Health, Social Care & Culture, Hackney Council and LGA Community Wellbeing Board member said:
“Alcohol affects every part of our communities from crime to poor health to litter and anti-social behaviour. That’s why it’s so important that councillors are equipped with the knowledge they need to start making the decisions which will help tackle alcohol misuse.
“I think many councillors will find this guide an invaluable resource with a background on central government alcohol policy and practical information on key alcohol issues.
“We mustn’t underestimate how important it is to get our policies on alcohol right. If we pull this off, every single person in our communities will benefit.”
The guide also points to success stories, including Suffolk’s innovative campaign to tackle super strength alcohol. It’s hoped the guide will give local policy makers the tools and advice they need to help them get to grips with alcohol misuse in their areas.
Download the free Guide to Alcohol for Councillors. At http://www.alcoholconcern.org.uk/publications/other-publications/guide-to-alcohol-for-councillors
Scotland’s Alcohol Strategy Interim Report
Trends in alcohol consumption and harm are moving in the right direction, but levels of harm in Scotland remain substantially higher than those in England, and much remains to be done.
These are among the main conclusions of the latest evaluation of the Scottish Alcohol Strategy, released by the Scottish government.
The report covers trends in price and affordability, alcohol sales and consumption, and alcohol-related harm. New chapters incorporating findings from the evaluation of the Licensing Act and the contribution of the economic downturn to recent falls in alcohol-related harms in Scotland are also included.
The main findings are:
Licensing Act evaluation
The activities outlined in the Licensing Act were, in the main, perceived to have been implemented as intended. Although compliance with the legislation was thought to be high, its overall impact is unknown.
Licensing Boards found it difficult to define and measure ‘overprovision’. Licensing Forums struggled to function effectively; understanding and addressing the public health objective has been challenging for Licensing Boards. Unless there has been a breach of legislation, Licensing Boards do not have the ability to withdraw existing licenses and are restricted to refusing new licenses (limiting the ability of Licensing Boards to reduce alcohol availability). Consequently, the Licensing Act, as yet, is unlikely to have a large impact on alcohol consumption in Scotland.
Alcohol consumption
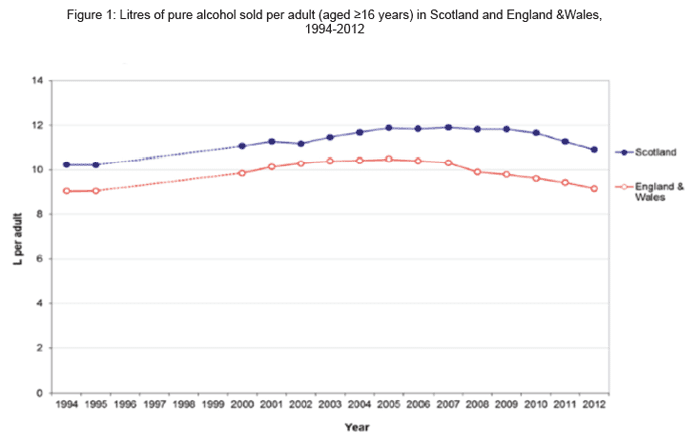
There has been a downward trend in the volume of pure alcohol sold per adult in Scotland since 2009, decreasing by a total of 8% between 2009 and 2012 (Figure 1).
Per adult sales in Scotland have been 19-21% higher than in England and Wales over the past five years. This is mostly due to higher off-trade sales in Scotland, particularly spirits.
The downward trend in self-reported weekly alcohol consumption, particularly since 2008, has been driven by young adults (aged 16-24 years) and those characterised as drinking at ‘harmful’ levels.
Declines have also been reported in the numbers of alcohol deaths and alcohol-related discharges from hospitals.
MESAS: 3rd Annual Report, December 2013
Contradictory claims in regard to Scots ban on multi-buys
Banning multi-buy promotions for alcohol, implemented in Scotland in October 2011 as part of the Alcohol Act 2010, has failed to reduce the amount of alcohol purchased, according to a new study. The research, conducted by the Behaviour and Health Research Unit – a collaboration between the University of East Anglia and the University of Cambridge – is published in the academic journal Addiction.
However, these findings are in contradiction to those of NHS Scotland, which suggested that the ban on multi-buys was working. As reported in UK Alcohol Alert Issue No 2 2013, a report from NHS Scotland claimed that a 2.6% decrease in the amount of alcohol sold per adult in Scotland was attributable to the ban.
Researchers at NHS Health Scotland and the University of Glasgow found that the 2010 Act, which included a ban on multi-buy promotions, was associated with a 4% drop in the amount of wine sold in Scotland’s supermarkets and off-licences, equivalent to almost 4.5 million bottles. The Act was also associated with an 8.5% decline in the amount of pre-mixed alcohol drinks (including alcopops) sold in Scotland, although these account for only 1% of the total alcohol market.
Mark Robinson, Public Health Information Manager at NHS Health Scotland and study lead, said:
“These findings show that the Alcohol Act has had the intended impact of reducing alcohol consumption in Scotland by placing restrictions on how alcohol is displayed and promoted. We know that some retailers responded to the multi-buy discount ban by selling individual bottles of wine for £3.33 instead of offering 3 bottles for £10.
“However, the incentive for people to buy more alcohol than they may otherwise have bought was removed and wine sales decreased.”
However, these claims are not borne out by the new study. Using detailed household purchasing data, the Behaviour and Health Research Unit researchers evaluated the impact of the policy on the volume of alcohol purchased as well as on consumers’ alcohol shopping patterns.
They found that the data as of June 2012 showed no evidence that the ban on multi-buys reduced the purchasing of beer, cider, wine, spirits, and flavoured alcohol drinks. In addition, it did not reduce the total amount of units of alcohol purchased.
They also found that the policy influenced shopping patterns for beer and cider, for which multi-buys had been used intensively. Scottish consumers started buying fewer products per shopping trip than they would have without the ban, but went out to buy beer and cider more frequently, leaving the overall amount purchased unchanged.
Lead author Dr Ryota Nakamura from UEA’s Norwich Medical School said:
“The industry appears to have responded to the ban by replacing multi-buy with simple price reduction, which made it possible for Scottish consumers to buy alcohol at a discounted price but with a smaller financial outlay. This might have mitigated the intended effects of the policy.”
Professor Theresa Marteau, from the University of Cambridge, said: “This study provides timely evidence on the seeming ineffectiveness of an intervention designed to reduce alcohol consumption.”
Professor Marc Suhrcke, also from UEA’s Norwich Medical School added: “More encompassing policy will be needed to achieve the goal of reducing excessive alcohol consumption and related harms. Partially banning price promotions leaves the door open for industry to just switch to other forms of price promotions, or indeed to reduce the overall price of alcohol. Imposing greater excise duties on alcohol and introducing minimum unit pricing have been shown to reduce alcohol consumption and associated harms. The Government has recently put on hold plans to introduce minimum unit pricing.”
Why the two research teams came to such different conclusions about the impact of the muliti-buy ban is not clear. However, there is agreement that the effectiveness of the ban has been undermined by alcohol retailers using other forms of price reduction to circumvent the ban on multi-buy discounts. multi-buy promotions for alcohol, implemented in Scotland in October 2011 as part of the Alcohol Act 2010, has failed to reduce the amount of alcohol purchased, according to a new study. The research, conducted by the Behaviour and Health Research Unit – a collaboration between the University of East Anglia and the University of Cambridge – is published in the academic journal Addiction.
However, these findings are in contradiction to those of NHS Scotland, which suggested that the ban on multi-buys was working. As reported in UK Alcohol Alert Issue No 2 2013, a report from NHS Scotland claimed that a 2.6% decrease in the amount of alcohol sold per adult in Scotland was attributable to the ban.
Researchers at NHS Health Scotland and the University of Glasgow found that the 2010 Act, which included a ban on multi-buy promotions, was associated with a 4% drop in the amount of wine sold in Scotland’s supermarkets and off-licences, equivalent to almost 4.5 million bottles. The Act was also associated with an 8.5% decline in the amount of pre-mixed alcohol drinks (including alcopops) sold in Scotland, although these account for only 1% of the total alcohol market.
Mark Robinson, Public Health Information Manager at NHS Health Scotland and study lead, said:
“These findings show that the Alcohol Act has had the intended impact of reducing alcohol consumption in Scotland by placing restrictions on how alcohol is displayed and promoted. We know that some retailers responded to the multi-buy discount ban by selling individual bottles of wine for £3.33 instead of offering 3 bottles for £10.
“However, the incentive for people to buy more alcohol than they may otherwise have bought was removed and wine sales decreased.”
However, these claims are not borne out by the new study. Using detailed household purchasing data, the Behaviour and Health Research Unit researchers evaluated the impact of the policy on the volume of alcohol purchased as well as on consumers’ alcohol shopping patterns.
They found that the data as of June 2012 showed no evidence that the ban on multi-buys reduced the purchasing of beer, cider, wine, spirits, and flavoured alcohol drinks. In addition, it did not reduce the total amount of units of alcohol purchased.
They also found that the policy influenced shopping patterns for beer and cider, for which multi-buys had been used intensively. Scottish consumers started buying fewer products per shopping trip than they would have without the ban, but went out to buy beer and cider more frequently, leaving the overall amount purchased unchanged.
Lead author Dr Ryota Nakamura from UEA’s Norwich Medical School said:
“The industry appears to have responded to the ban by replacing multi-buy with simple price reduction, which made it possible for Scottish consumers to buy alcohol at a discounted price but with a smaller financial outlay. This might have mitigated the intended effects of the policy.”
Professor Theresa Marteau, from the University of Cambridge, said: “This study provides timely evidence on the seeming ineffectiveness of an intervention designed to reduce alcohol consumption.”
Professor Marc Suhrcke, also from UEA’s Norwich Medical School added: “More encompassing policy will be needed to achieve the goal of reducing excessive alcohol consumption and related harms. Partially banning price promotions leaves the door open for industry to just switch to other forms of price promotions, or indeed to reduce the overall price of alcohol. Imposing greater excise duties on alcohol and introducing minimum unit pricing have been shown to reduce alcohol consumption and associated harms. The Government has recently put on hold plans to introduce minimum unit pricing.”
Why the two research teams came to such different conclusions about the impact of the muliti-buy ban is not clear. However, there is agreement that the effectiveness of the ban has been undermined by alcohol retailers using other forms of price reduction to circumvent the ban on multi-buy discounts.
A decade of alcohol strategy: What has been achieved?
Calls to curb problem drinking have been made for years, but are the Government’s policies having any impact on levels of consumption?
James Morris examines a decade of alcohol strategy
The first national level strategy for addressing alcohol misuse was introduced just under ten years ago. However, this relatively new era of Government alcohol policy has so far failed to instigate the national measures needed to affect real change.
Things have been shifting, with many local areas now prioritising action to address the significant harm that alcohol misuse causes. Yet to really turn the tide, strong national and local-level action needs to be sustained simultaneously.
Local-level action without effective national policy is akin to trying to empty a plugged bath while the taps are still on.
The Government’s latest strategy, published in 2012, was to be applauded solely for its commitment to ‘introduce a minimum unit price’. But huge gaps remained, particularly in relation to improving key health and treatment interventions needed to reach the millions of at-risk and dependent drinkers. Minimum pricing is no panacea, but the evidence shows price is the leading determinant of overall consumption. Since 1980 alcohol is at least 45% more affordable – and the stark rise in consumption directly correlates.
Unfortunately, the recent strategy included no action plan, measurable outcomes or commitments to support or strengthen local level action on health and treatment. Its foreword used the crime agenda to justify minimum pricing, labelling problem drinkers as ‘drunks’ and ‘binge drinkers’. Whilst these problems do exist, we cannot ignore the huge burden of still rising hospital admissions associated with long term health conditions. The French may have a more desirable social attitude to alcohol, but their liver cirrhosis and dependency rates are not to be admired.
The strategy’s only other firm commitments focused on ‘re-balancing’ the licensing act. However, such action targets a trade already the subject of significant pressure. Well-run pubs should perhaps be viewed as part of the solution, not the problem. It is the ‘stack it high, sell it cheap’ approach of the off-trade that has fuelled ‘the rise of harmful home drinking and ‘pre-loading’.
But what of the newer Government-backed initiatives, like the ‘Responsibility Deal’ and the increasing permeation of health messages to the general public? The Responsibility Deal’s alcohol pledges may have some value, but they do not deliver on what is most effective. The Deal’s problems have been well documented and Asda recently announced it was pulling its commitment to remove alcohol from the front of its stores after competitors failed to follow suit. The pledges that look likely to be achieved are mainly focused around increasing unit labelling and ‘educational approaches’, which are not enough to affect actual behaviour change.
I regularly ask people what health messages they can recall around alcohol – confused guidelines and broad ‘drink responsibly’ phrases often come up. Isolated messages simply telling us to ‘drink safely’ are unhelpful at best, because ‘responsible drinking’ is such a subjective notion. Most at-risk drinkers don’t have a good understanding of the units they are drinking and how these relate to the guidelines – the majority believe they actually are ‘drinking safely’.
So whilst some improvements are being made in understanding units, guidelines and alcohol risks, there is a long way to go into converting this into actual behaviour change. The most far reaching health messages come via Drinkaware, the industry-funded alcohol education organisation who recently received a rather critical independent review. Its own recent performance report also showed a mixed performance in meeting its own targets. Perhaps most worryingly, unpublished research by Southbank University suggested some of its messages appeared to contribute to increased drinking.
This is not to say the ‘Responsibility Deal’ or Drinkaware do not have a role to play. Industry profit motives and efforts to reduce harm may often be in conflict, but not always. For instance, the Responsibility Deal’s pledge to remove one billion units by 2015 could deliver population-level health gains, even if shifting sales to lower strength drinks leads to higher profits from saved duty. But crucially, these initiatives are not going to achieve the deal’s core aim of “a culture of responsible drinking” unless we take strong action on price, availability and marketing.
An alternative alcohol strategy named ‘Health First’ was produced earlier this year by an alliance of health bodies. It aimed to detail an evidence-led approach for the Government to take, from which current policy is some way off. We may be starting to see some positive changes to our £21 billion a year drink problem and cultures do take time to shift. But the issue of minimum pricing is not going to go away. As long as cheap alcohol permeates our society, new generations will be developing alcohol problems on a scale that should be prevented.
James Morris is a Director at the Alcohol Academy
Reproduced by kind permission of www.westminster-briefing.com http://tinyurl.com/klkgk3k
These are the views of James Morris and do not neccesarily reflect those of the Institute of Alcohol Studies
Wales: Chief Medical Officer launches alcohol awareness pack
Wales’ top doctor, Ruth Hussey, visited Swansea University to launch a package of advice helping counsellors to spot signs of alcohol misuse in students.
The Welsh Government gave £15,000 towards the development of the Alcohol in Higher Education Toolkit, consisting of guidance designed by a group comprising the Welsh Government, the NUS and Drinkaware, in conjunction with Cardiff University.
It contains a comprehensive range of information for student welfare services, giving practical advice on addressing alcohol misuse.
The toolkit offers:
- best practice guidelines for addressing alcohol misuse
- guidance on developing appropriate alcohol policy
- information on student support services and addressing the social environment
The toolkit was trialled in four universities across Wales: University of Wales – Trinity St David, Aberystwyth University, University of Wales Newport and the University of Glamorgan, and was then evaluated by Cardiff University. In July 2013, the toolkit was rolled out to all remaining universities in Wales.
Launching the toolkit, Dr Ruth Hussey said:
“I am very pleased to launch the Alcohol in Higher Education Toolkit. This is not a matter of lecturing young people about how much they drink. Rather it is a way of helping to recognise alcohol misuse and reducing the impact.
“Excessive alcohol consumption among university students has been linked to educational difficulties, psychosocial problems, antisocial behaviours and drink-related injuries.
“This toolkit has been produced to give student welfare services practical advice on addressing alcohol misuse.
“It aims to offer best practice guidelines for addressing alcohol misuse, gives guidance on developing appropriate alcohol policy and provides information on student support services and ways of addressing the social environment.”
The Toolkit can be accessed here: http://wales.gov.uk/topics/health/improvement/index/toolkit/?lang=en
New hard-hitting alcohol health campaign launches in the North East
Alcohol likened to tobacco, asbestos
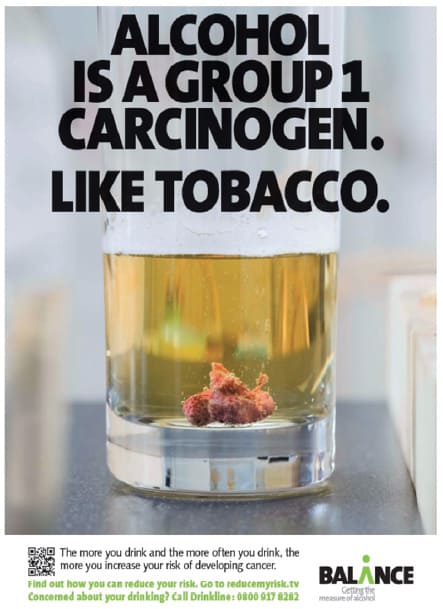 Drinkers are being warned that alcohol is in the same cancer-causing category as tobacco smoke and asbestos as part of a new hard-hitting health campaign, launched in the north east of England as part of Alcohol Awareness Week.
Drinkers are being warned that alcohol is in the same cancer-causing category as tobacco smoke and asbestos as part of a new hard-hitting health campaign, launched in the north east of England as part of Alcohol Awareness Week.
Balance, the North East Alcohol Office, is aiming to raise awareness of the links between alcohol and cancer – with alcohol responsible, it says, for around 12,500 cases of cancer each year in the UK.
There are seven types of cancer that are linked to alcohol; mouth cancer, pharyngeal cancer (upper throat), oesophageal cancer (food pipe), laryngeal cancer (voice box), breast cancer, bowel cancer and liver cancer. And, Balance says, it isn’t just heavy drinkers who are at risk – ‘the more you drink, and the more often you drink, the greater the risk’.
Studies have shown that:
- Drinkers are three times more likely to develop cancers of the mouth and throat by drinking above the recommended limits
- Regularly drinking just above the recommended guidelines increases the risk of getting breast cancer by around 20%
- Alcohol is one of the main risk factors for liver cancer
In the latest Balance public perception survey carried out across the North East only 21% of people stated that alcohol greatly increases the risk of cancer – with 18% believing that alcohol doesn’t increase the risk at all. There were also low associations with alcohol and some cancer types. When questioned, over a third (34%) didn’t associate alcohol with breast cancer, almost one in four (23%) people didn’t associate alcohol with mouth and throat cancer and one in five (21%) didn’t associate alcohol with bowel cancer.
The campaign will launch across TV screens and it is set to be one of the hardest-hitting regional health campaigns for alcohol to date. The film shows a man in the kitchen about to prepare a meal. As he is doing this you see him reach into the fridge for a bottle of lager, which he then pours into a glass. As he starts to drink the lager an object becomes visible in the bottom of the glass. The more he drinks, the bigger the object gets. In one of the final shots, the film depicts the tumour sliding towards his mouth.
Colin Shevills, Director of Balance, explains: “We appreciate that this is quite an uncomfortable film to watch but evidence tells us that hard-hitting campaigns work and we want to highlight the harms that can be caused by drinking too much, too often. Unlike tobacco, very few people associate alcohol with cancer and we need these perceptions to change.
“We need to continue to raise awareness of the potential health impacts caused by alcohol. Alcohol is linked to more than 60 different medical conditions, including liver disease, cancer, osteoporosis, stomach ulcers, raised blood pressure, stroke and dementia.”
Sarah Williams, health information officer at Cancer Research UK, said: “Hard hitting, memorable campaigns like this help to highlight the risks of drinking alcohol. And remind us that it can cause serious health problems, including cancer – causing around 12,500 cases every year in the UK. It isn’t just heavy drinking that increases the risk. But the more you cut down on alcohol, the better – try making every other drink something soft, or making a pact on alcohol-free days with your partner and friends.”
Alcohol Harm: Attention switches to middle aged and elderly though binge drinkers remain disproportionately young
Though young people are still more likely than older age groups to binge drink periodically, it is the middle aged and elderly who are now more likely to drink frequently and in whom the largest burden of alcohol-related disease is now being found.
These are the conclusions of the latest Office of National Statistics report on adult drinking in Great Britain and the Dr Foster analysis of alcohol-related hospital admissions.
Adult Drinking in Great Britain
The latest ONS survey results reflect the continuing decline in the overall level of alcohol consumption, but also show that, despite that decline, heavy episodic drinking is still prevalent in young people. The main findings of the survey are:
In 2012, 58% of adults (people aged 16 and over) living in private households in Great Britain drank alcohol at least once in the week before being interviewed. This proportion has been declining both for men and women. Between 2005 and 2012 the proportion of men who drank alcohol in the week before being interviewed fell from 72% to 64%, and the proportion of women fell from 57% to 52%.
The proportion of adults who drank frequently (those who drank alcohol on at least five days in the week before being interviewed) has also been declining. Between 2005 and 2012 there was a fall from 22% to 14% in the proportion of men who were frequent drinkers, and from 13% to 9% in the proportion of women. In 2012, people aged 65 and over were most likely to have drunk frequently, both for men (23%) and women (14%).
Young people (those aged 16-24) were more likely to have drunk very heavily (more than 12 units for men and 9 units for women) at least once during the week (27%), with similar proportions for men (26%) and women (28%). Only 3% of those aged 65 and over were very heavy drinkers.
Very heavy drinkers were five times more likely than other drinkers to have drunk strong beer/ stout/lager/cider, and more than twice as likely to have drunk spirits or liqueurs, on their heaviest drinking day in the week before interview.
Smokers (25%) were more than twice as likely as non-smokers (11%) to have drunk very heavily at least once during the week.
Hospital admissions
Dr Foster, a leading supplier of information to the health service, in its analysis of alcohol and other drug hospital admissions, stresses that these are now increasingly a middle age issue. The figures show that alcohol or drug problems account for just under one in five of all emergency admissions in 40-44 year olds, the highest proportion in any age group. Moreover, the average age of admissions for long term alcohol and drug problems is rising.
Online marketing threat to young adults
There should be tighter regulation around alcohol marketing aimed at young people who use social network sites, according to psychologist Professor Christine Griffin of the University of Bath.
Professor Griffin, who is part of the UK Centre for Tobacco and Alcohol Control Studies (UKCTAS), found that young people are vulnerable to marketing tactics on online sites such as Facebook and do not always recognise this as advertising.
She worked with academics from Massey University in Auckland and Wellington, New Zealand, researching how 18 to 25 year olds respond to online marketing of drink brands.
The amount of money large alcohol companies are devoting to digital marketing is increasing rapidly. The study found that online alcohol marketing aimed at young adults is widespread, highly dynamic and takes an ever-expanding range of forms as new digital and mobile technologies develop. Young people tend to view targeted alcohol marketing via social media as useful and informative, seldom recognising it as advertising. However, online alcohol marketing is pervasive across a range of social media platforms, and encourages a culture of intoxication or ‘extreme drinking’ amongst young adults.
Professor Griffin shared her findings with the all-party parliamentary group on alcohol misuse in the Houses of Parliament.
She said: “Traditional behaviour change approaches to tackling young adult’s excessive alcohol consumption are highly individualised, and unlikely to succeed in this context. A wider range of policies and safer drinking initiatives that target the cultural norm of drinking to intoxication are required.
“Current attempts at health promotion are outmoded, and need to employ social media and mobile technologies more effectively to challenge the messages from alcohol marketing.
“We need to examine corporate practices and digital alcohol marketing strategies – and implement effective alcohol policies in the light of this information.”
The three-year study, which involved interviews with young social network users, found that sites such as Facebook play an important role before drinking, during drinking, and following drinking episodes and that sharing photos is particularly important.
She said: “The sites reinforce the idea that drinking is about fun, pleasure and socialising. Alcohol brands become an integral part of young people’s everyday lifestyles, reinforcing the widespread culture of intoxication.
“But despite the vast amount of alcohol products, events and marketing on the internet, and particularly on Facebook, this content was not always viewed as marketing. For many participants, only Facebook ads in the sidebar were interpreted as marketing. Social media therefore offers important opportunities for alcohol marketing to young people – and alcohol companies have been quick to recognise this.
“Every click and interaction with an alcohol product page on Facebook gives data about the individual. This information is used to present users with marketing that is personally tailored to them, that is targeted advertising based on your identity, interests, peer network, attendance at events, or location.
“The regulation of alcohol marketing should include new media and digital marketing, and be flexible to include new and evolving marketing activities.”
Professor Griffin said keeping track of digital alcohol marketing strategies and how they are used by different groups of young people is a major endeavour. She said: “There is a role for research on whether digital alcohol marketing increases young people’s alcohol consumption – but it’s equally (if not more) important to investigate how these marketing strategies are taken up and how they engage young people and infiltrate their everyday social lives via social media – whether they are even seen as advertising for example. Then can we consider more effective ways of challenging such practices.”
Neknomination: extreme drinking game goes viral
Warnings about the possibly harmful impact of social media such as Facebook and YouTube gained added force from the sudden emergence of a competitive drinking game generally known as ‘Neknomination’. The game, which has become a global phenomenon, thanks to social networking sites, has the potential to kill participants or third parties.The name ‘Neknomination’ is derived from ‘neck your drink, nominate another’, and it involves participants filming themselves drinking as much alcohol as they can as quickly as possible while doing something outrageous and often dangerous. The video is then posted on-line with a challenge to friends to out-do the stunt. Participants who pass out before being able to issue the challenge to their friends are ridiculed online.
There is some difference of opinion as to where the craze originated, but the global reach of social media means that it is rapidly spreading around the world. Incidents have been reported in Australia, South Africa, Canada, the UK and Ireland. Stunts have included biting off the head of a chicken, and being held by the ankles to drink alcohol that had been poured into a lavatory.
Other filmed stunts have been even more bizarre or dangerous, as participants try to out-do their rivals. One man was filmed nailing his testicles to a table while he ‘chugged’ beer. Others have drunk alcohol and then been filmed drinking non-alcoholic liquids such as urine or lubricating oil. Yet others have been filmed drinking while dangling from a helicopter or doing dangerous stunts in cars or motorcycles.
In Northern Ireland, a Neknomination Facebook page was set up for video postings and received over 10,000 ‘likes’ in less than a week. In Australia, a Facebook page, ‘The Best Neknominate Videos’, attracted more than 190,000 ‘likes’ before it was taken down.
The Northern Irish site has also been closed down and converted into an alcohol awareness resource following the reported deaths of two young Irishmen which are being attributed to the craze. One of them, a teenager, is reported to have deliberately jumped into a river, where he drowned.
Councils issue warning
Social media giants, Twitter and Facebook, should introduce health warnings to tackle the ‘Neknomination’ craze, according to the Local Government Association (LGA). The LGA, representing almost 400 councils in England and Wales, has urged the duo to post prominent messages on their sites, spelling out the risks. These could be along the lines of the shock cautions emblazoned on cigarette packets, it suggests.
Councils across the country are launching internet safety campaigns providing links for parents, carers and young people who use the internet, and offering advice and support over alcohol-related issues. Neknomination warning notices have been requested by schools so they can be put up on notice boards and read out at assemblies.
Cllr Katie Hall, Chair of the LGA’s Community Wellbeing Board, said:
“This is an utterly reckless and totally irresponsible craze which has tragically claimed lives. More should be done to highlight the dangers and persuade people not to participate.
“We believe social media operators have a responsibility to provide health warnings to user groups and individuals.
“The LGA is looking for these corporations to show leadership ¬and not ignore what is happening on their sites. We are urging Facebook and Twitter executives to sit down with us and discuss a way forward which tackles this issue head-on.
“Neknomination is at the extreme end of a very long wedge. Each year, there are over 1.2 million alcohol-related hospital admissions, over 8000 deaths and 17 million working days are lost. The annual cost to the NHS is £3.5 billion. A quarter of acute male admissions to hospital are alcohol induced.”
Case studies
Boston Borough Council, Lincs, are encouraging Neknominees to contact their community safety team. Main secondary schools are posting warning notices up and mentioning it in school assemblies.
Sevenoaks District Council is launching an internet safety campaign to provide links and advice for parents, carers and young people who use the web.
Worcestershire County Council has called for people not to participate. Alcohol-related illness cost Worcestershire’s NHS more than £25 million and about 60 people die every year in Worcestershire where alcohol is a contributing factor.
– See more at: http://www.local.gov.uk/web/guest/media-releases/-/journal_
 Doctors offered guide to workplace alcohol and drug problems
Doctors offered guide to workplace alcohol and drug problems
The British Medical Association (BMA) has published new guidance to help doctors better understand and support patients and employers in tackling alcohol and illicit drug use in the workplace.
The guidance recognises the prevalence of alcohol and drug misuse among people in employment, and the impact on employers in terms of absenteeism and behavioural issues. Doctors also need to understand the employment aspects of drug and alcohol misuse and how patients can access fitness-to-work advice and reports, the association says.
Alcohol and Drugs in the Workplace: The Role of Medical Professionals points out that alcohol and illicit drug use is prevalent in those who are in work and, as such, is a significant issue for the workplace and is a growing concern for employers. Individuals in employment are more likely to drink frequently, compared to those who are unemployed. Individuals in managerial and professional occupations drink more frequently than those in routine and manual occupations. There were 8,748 alcohol-related deaths in 2011, and 1,785 linked to illegal drug use. The signs of alcohol and drug misuse are often more commonly spotted in the workplace, where colleagues and employers notice the absenteeism, poor performance or productivity and inappropriate behaviour it can cause.
Recognising misuse
BMA Occupational Medicine Committee Chair, Paul Nicholson, said: “Only around one in seven workers have access to a qualified occupational physician, with many relying on their GP or hospital specialist for advice relating to fitness for work.
“For this reason it is fundamental that all doctors understand the risks associated with alcohol and drug use in people who work. Medical professionals should also consider a patient’s occupation when prescribing medication that might affect their fitness for specific types of work, particularly those patients who drive, operate machinery or work at heights.”
The BMA says managers and supervisors should be trained to recognise alcohol and drug misuse problems among their staff and such employees should have access to occupational health services. Medical professionals who support workplaces could provide this training to staff, the association says.
Intervention techniques
It advises doctors who are asked for advice by an employer to first establish the capacity in which they are being asked to comment, and also to seek to understand the employer’s alcohol and drug policy, which may apply across the workforce or just to those in safety critical roles. The guidance adds that workplaces can provide venues for health education and the opportunity to identify individuals with drug problems.
The BMA Report – Doctors offered guide to drink-drug work risk – can be downloaded from the BMA website using the following link:
http://bma.org.uk/news-views analysis/news/2014/january/doctors-offered-guide-to-drink-drug-work-risk
Increasing problem of counterfeit alcohol – ‘White Van Man’ implicated
Further evidence of the problem of counterfeit and smuggled alcohol has been provided in Peterborough and Leeds.
In Peterborough, a retailer has had its licence to sell alcohol revoked after officers seized over 50,000 litres of smuggled alcohol. Trading Standards have requested a review of the licence after the illicit goods were seized at two of its cash and carry units. An application to review the firm’s alcohol licence has been sent to the city council by Trading Standards with a recommendation that it is revoked.
The application stated that, in total, 51,506.46 litres of assorted beer and cider and 9.5 litres of spirits were seized, and officers were satisfied that due to the proprietor’s inability to produce invoices or receipts to prove duty payment, that excise duty had not been paid on the goods. The revenue due on the seized goods, including VAT, was £66,167.48. The goods were forfeited.
The raids resulted in a suspected smuggling racket, estimated to have cost the taxpayer around £6 million, being smashed.
Leeds White Van Man
In Leeds, following a rise in the number of counterfeit alcohol investigations, West Yorkshire Trading Standards Service and West Yorkshire Police issued a warning to traders to avoid the temptation of buying alcohol from a ‘white van man’.
Recently, West Yorkshire Trading Standards Service has prosecuted a number of licensees. The defendants in each of the cases had bought counterfeit alcohol from a ‘white van man’ at ‘rock bottom’ prices and the retailers were unable to provide sufficient information to trace the supplier.
The cheap products being sold by unscrupulous suppliers may cause a health risk to consumers. Tests carried out on Drop Vodka, Activ Vodka and on counterfeit Stolichnaya Vodka have found Chloroform, Isopropanol, Methyl Ethyl Ketone, Methyl Iso Butyl and Dichloromethane. Trading Standards have also seized Bulgarian white wine that was illegally labelled as ‘Soave’ and a product illegally described as ‘Sambuca’.
Criminal rackets
As reported previously in UK Alcohol Alert, Her Majesty’s Revenue and Customs estimates that fraud against alcohol duties may have cost the Exchequer up to £1.2 billion in 2009 – 10. The fraud is carried out primarily by organised criminals who exploit weaknesses in the supply chains of alcohol producers, wholesalers and distributors to divert goods onto the UK market without paying the taxes that are due.
Opportunities for excise fraud emerged effectively with the creation of the European Union (EU) single market on 1 January 1993. Until that time, the Department and customs authorities in other Member States had established tight control of excise goods to ensure duties were paid on the goods produced. Once the European single market was established, businesses were legally free to move goods around the EU, and alcohol could be held in warehouses on a duty suspended basis until they were dispatched.
As the Peterborough case suggests, there is an additional problem of counterfeit alcohol produced from illegal distilleries. An explosion which killed five men and severely injured a sixth on an industrial estate in Boston, Lincolnshire was found to have occurred in an illegal distillery operated by Lithuanian migrant workers. Police investigating the incident discovered a filtration plant used for an illegal alcohol distilling process, along with three lorry-loads of counterfeit vodka, falsely labelled as Smirnoff. Mass migration into the UK has resulted in approximately 25% of the residents of Boston now coming from Eastern Europe, and it seems that it is largely foreign migrants who are behind the growth in the illegal alcohol trade, which is not restricted to Lincolnshire.
In the Spring of 2011, Her Majesty’s Revenue and Customs (HMRC) carried out raids to find out who was buying and selling the counterfeit vodka and to try to stop it reaching store shelves. As well as Boston, the raids also took place in Peterborough in Cambridgeshire, St Albans in Hertfordshire and Newcastle. In 2010, an illegal distillery run by Polish migrants was found in Hackney in north London.
Nottinghamshire Alliance Against Violence
Nottinghamshire Police have launched a new campaign to tackle violent crime, with the main focus on alcohol-related violence. The campaign forms part of the police strategy on violent crime and encompasses hate crime, robbery, domestic violence, and crime which takes place during the night time economy and in public spaces.
Although we have seen an overall reduction in crime in recent years, numbers of violent crimes have started to rise. Last year, between July 2012 and June 2013, there were 13,217 instances of violent crime. Of these 7,106 resulted in injury.
Assistant Chief Constable Simon Torr said:
“Nottinghamshire has much to offer on a night out, it is a vibrant city and there are lots of good bars and clubs. We want people to come and have a good time and not have their night ruined because they have become a victim or an offender of violent crime…A lot of the issues are related to alcohol. Our campaign and our activity will focus on this.”
Mr Torr stressed that there are real issues in Nottinghamshire with alcohol and, particularly, ‘pre-loading’, when people consume alcohol and possibly get drunk even before they go out.
Mr Torr said: “Our figures show that people who ‘pre-load’ are 2.5 times more likely to be involved in violence as a victim or an offender. They are also four times more likely to consume over 20 units in a single night.
“Worryingly 50% of 18 – 35 year-olds pre-load on a Friday or Saturday night.
“People need to take greater responsibility for themselves and their friends to reduce the likelihood of them becoming injured, a victim or involved in violence.
“Drinking so much that you can’t think clearly makes you vulnerable and more likely to become a victim of crime, be injured or be involved in violence.”
The campaign will employ a range of measures and will include licensing teams carrying out checks, patrols of violent microbeats, offender management, repeat victim focus, engaging with neighbourhoods and communities, welcoming people coming into the city at bus and train stations, engaging with hen and stag party groups at hotels, a lot of preventative work and linking in with students.
There will also be an alcohol diversion scheme, when police can offer an alcohol referral course for people given a ticket for being drunk and disorderly. This reduces the cost of the fine they have to pay and, hopefully, helps to change their behaviour.
There will also be ‘naming and shaming’ of anyone who is charged with alcohol-related or violent crime and it is hoped that this will have a deterrent effect.
Podcast
Our monthly podcast features interviews with experts from across the sector.
Gambling industry harms and parallels with the alcohol world
Will Prochaska –
Coalition to End Gambling Ads