In this month’s alert
Editorial – February 2019
Welcome to the February 2019 edition of Alcohol Alert, the Institute of Alcohol Studies newsletter, covering the latest updates on UK alcohol policy matters.
This month, new alcohol health statistics expose growing divides in age and location throughout England. Other articles include: private funding keeps family drug and alcohol courts alive, new study finds Netflix and Amazon Prime ads are major global drivers for young people’s alcohol consumption, and journalist Olivier van Beemen’s new book exposes Heineken’s business practices in Africa.
Please click on the article titles to read them. We hope you enjoy this edition.
COVER STORY – New alcohol stats expose growing divides in age and location
Older drinkers and northerners suffer most from alcohol-related harms
05 February 2019 – Two new datasets on the health effects of alcohol consumption in England reveal huge and growing disparities in drinkers’ outcomes, with older people and those living the north worst off.
Both NHS Digital’s ‘Statistics on Alcohol England 2019’ and Public Health England’s ‘Local Alcohol Profiles for England (LAPE): February 2019 update’ found that while overall levels of morbidity and mortality remained largely flat, the geography and demography of alcohol-related harms fall disproportionately on certain groups.
In 2017/18, there were 1.2 million estimated admissions where the primary reason was linked to alcohol in England (broad measure), a slight increase on 2016/17 (3%), yet four out of every five (83%) of patients was aged over 45 years (illustrated).
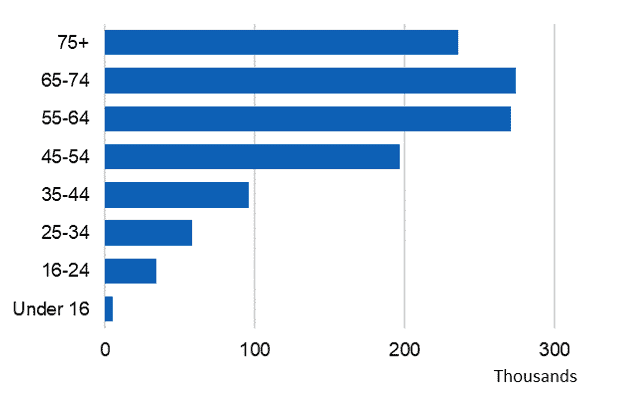
Hospital admissions (broad measure) |
As for the narrow measure, there were 337,900 admissions where the main reason for admission was attributed to alcohol – also slightly higher than last year (337,110) – yet when split by age, NHS Digital observed that ‘the number of admissions rises with age up until 55–64 and then falls’ (illustrated).
Hospital admissions (narrow measure) |
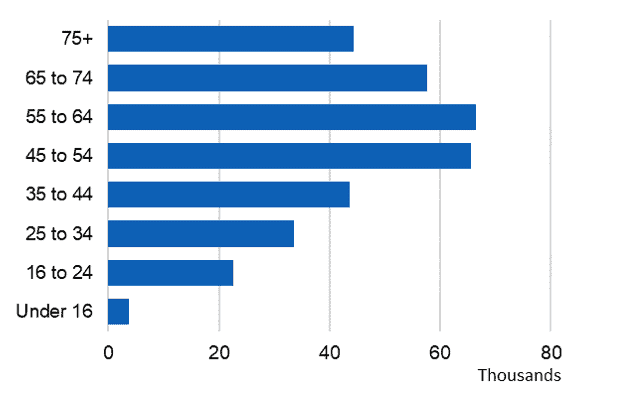
69% of patients were aged over 45. LAPE data showed that the majority of admissions were for cardiovascular disease (52%), and a sizeable proportion (17%) were for mental and behavioural disorders due to alcohol (illustrated).
Chronic partially-attributable conditions |
Alcohol mortality figures told a similar story. A 6% increase in alcohol-specific deaths (from 5,507 in 2016 to 5,843 in 2017) masked the fact that split by age, the number of deaths in every age cohort increases up to 50–59 years of age before falling. 78% of deaths were in the age range 40–69. Almost a quarter of admissions were for cancer and 23% were for unintentional injuries.
Furthermore, when split by region, age-standardised death rates were highest in the north and lowest in London and the south (illustrated). A similar north/south divide emerges for hospital admissions – NHS Digital found that Blackpool and Salford (in the north west of England) had the highest alcohol admissions rates, whereas Wokingham (in the south east) had the lowest rates.
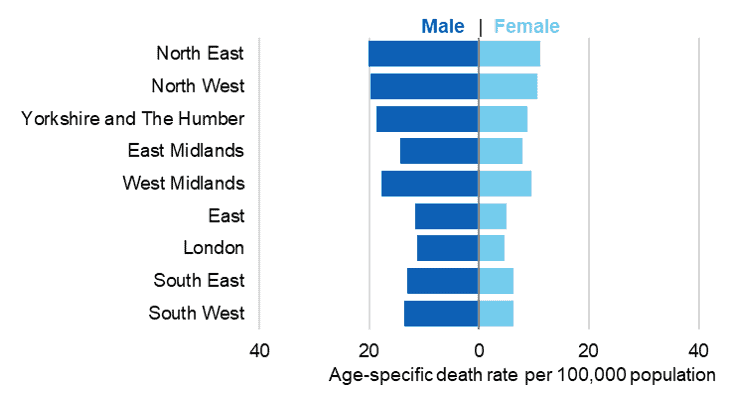
Age-specific death rates, by region |
Older drinkers were also most likely to drink at increased or higher risk of harm; that is, over 14 units of alcohol in the last week – Split by age, both men and women 55–64 years of age were most likely to do so in 2017 (36% and 20% respectively). This statistic is set against a backdrop of a falling proportion of increased or higher risk drinkers between 2011 and 2017. 55–64 year-olds were also most likely to drink in the last week (72% and 63% respectively), and those aged 50–74 years of age spent the most on alcohol in England, with 65–74 year-olds splashing out £10.60 per week in 2017, £1.90 above the national average weekly spend of £8.70. In terms of affordability, Stats on Alcohol England found that beverages are becoming ever more affordable – in 2018 alcoholic drinks were 64% more affordable than they were in 1987.
There was a typically positive correlation between alcohol-specific death rates and areas of deprivation for both sexes – the more deprived an area, the higher the (alcohol-related) mortality rate.
Yet, the proportion of adults usually drinking at increased or higher risk of harm was highest in higher income households – this suggests that higher levels of alcohol harm in poorer households is down to several factors, not consumption levels alone.
Commenting on the figures, chair of the Alcohol Health Alliance, Professor Sir Ian Gilmore said:
‘These figures send a strong message to the Government that an evidence-based approach to tackling alcohol harm is long overdue if they are truly committed to tackling health inequalities.’
Grades and occupation linked to drinking habits
School leavers and managerial types stand out among respondents
05 February 2019 – Social-grade and education attainment may be the strongest socioeconomic predictors for alcohol consumption frequency and volume in England, according to a study of more than 50,000 drinkers published in PLoS One.
Researchers from University College London, the University of Sheffield, and Newcastle University found that those in so-called ‘high-flying jobs’ were among the most frequent drinkers, and that those whose highest educational achievement was at advanced level (A-level) were most likely to binge drink.
The researchers used the Alcohol Toolkit Study to collect data on 57,807 drinkers in England over a four-year period, in a study aimed to ‘gain a better understanding of the complex relationships of different measures of social position, educational level and income with alcohol consumption’. The research team measured the following indicators: social-grade (based on occupation), employment status, educational qualifications, home and car ownership and income.
They found that the strongest predictor of drinking frequency was social-grade – those in the two lowest occupation categories had fewer drinking occasions compared with those in professional-managerial positions. They also found that the strongest predictor of amount consumed and binge drinking frequency was lower educational attainment – those whose highest qualification was an A-level drank significantly more than those with a university qualification.
NICE updates guideline on alcohol education in schools
NICE is updating its guideline on alcohol interventions in secondary and further education
08 February 2019 – New draft recommendations will support the Department for Education’s (DfE) plan to make alcohol education a compulsory component of personal, social and health education (PSHE) in all state-funded schools in England from September 2020.
The guideline, developed with Public Health England, advises a positive approach to alcohol education; inviting classroom discussion and wider school policies to embed a ‘whole-school approach’ to PSHE.
Data suggests that alcohol consumption among young people has reduced in recent years. However, NICE’s independent guideline committee recognised that risky drinking can still be an issue for young people and that some pupils may be more vulnerable to alcohol misuse.
Therefore, the draft guideline also covers targeted interventions for pupils identified as being most at risk. It says these interventions should be tailored to individuals’ needs and should avoid stigmatising the pupils involved.
Healthy decisions
Joanne Boyd, a member of the guideline committee and a trainer at Humankind, which provides the County Durham Drug and Alcohol Recovery Service, said: “For young people to leave school with healthy lives ahead of them, they need to be educated so they can make informed choices and be aware of the consequences of alcohol consumption.
“This guideline will help ensure that alcohol education isn’t a one-off topic, and that schools provide age-appropriate and accurate information.”
Professor Gillian Leng, deputy chief executive of NICE, said: “There are many examples of schools that deliver very good alcohol education. The updated NICE guideline reinforces best practice and helps schools provide alcohol education that fits into the new era of PSHE.
“We have also made a number of research recommendations to help develop the evidence base for the future, in an area that is vital in helping young people make informed, healthy decisions.”
A public consultation on the updated guideline runs until 22 March. Final guideline is due to be published in August 2019.
CMO Dame Sally Davies to stand down in September
Oversaw the implementation of new alcohol guidelines
08 February 2019 – The government’s chief medical officer, Dame Sally Davies, will step down at the end of September after nine years in the role, the Department of Health and Social Care has announced.
Davies will leave the civil service to become master of Trinity College at the University of Cambridge. Davies first joined the civil service in 2004 as director general of research and development for the NHS, where she set up the National Institute for Health Research – the research arm of the health department that manages a research budget of around £1bn a year.
She then moved on to become the first ever female chief medical officer for England in June 2010, taking over from Sir Liam Donaldson.
In January 2016, she ushered in the new alcohol guidelines, which saw the recommended weekly alcohol limit lowered from 21 to 14 units for men, matching women. The guidelines also warned that drinking any level of alcohol increases the risk of a range of cancers, a result of better knowledge of the links between alcohol and cancer, that were not fully understood in the original guidelines when they first came out in 1995.
She said: ‘I want to pay tribute to the outstanding clinicians, scientists and public servants who have supported me in this role – men and women who are working tirelessly to improve the health of the nation.’
Cost of alcohol’s impact on wellbeing sparks debate
Study demonstrates perils of quantifying alcohol’s psychological toll
13 February 2019 – Media coverage of a new study attempting to express the impact of alcohol on mental wellbeing in financial terms has generated controversy, with critics arguing that its findings have been misinterpreted. The paper was published in the journal PLOS One earlier this month by a team of researchers led by the University of Oxford’s Chenlu Li and Cardiff University’s Simon Moore. Using a large UK database containing information on over 240,000 individuals, they found that people who drink more tend to suffer higher levels of depression and neuroticism. As a way of measuring the size of this relationship, they estimated that the increase in these symptoms associated with each extra gram of alcohol consumed each day was the same as the increase (in the same symptoms) associated with a £210 decrease in a person’s annual income.
These findings received a lot of newspaper attention, with The Times reporting that ‘Downing a bottle of wine a week costs, gulp, £2,400 a year in lost quality of life’. Yet such headlines were condemned as ‘very exaggerated’ by Sir David Spiegelhalter on the BBC’s More or Less programme. They might be seen as misleading for two reasons.
First, the estimated costs represent an average across different levels of alcohol consumption, which may or may not reflect the cost to any given person. Instead of there being a linear relationship between alcohol consumed and the impact on depression and neuroticism, it is possible that the impact of moving from one to two bottles of wine a week is considerably less than this, and the impact of moving from four to five bottles considerably more.
Second, the study reports correlations between alcohol consumption and mental wellbeing, but does not claim that these relationships are causal. It is possible, for example, that part of the reason why heavier drinkers have higher depression and neuroticism is that those with worse mental health to begin use alcohol to self-medicate. To the extent that this is the case, it means that the direct effect of drinking more alcohol will be less than the reported £2,400.
The episode appears to demonstrate the methodological difficulty of producing a robust estimates of the impact of alcohol on mental wellbeing. Indeed, Professor Moore appears to see the paper as an opening step in an ongoing process, saying ‘I welcome criticism that helps us develop these methods and helps the scientific community develop to better capture the true costs of alcohol’.
Donors step in to back family drug and alcohol courts
Adapted from BBC News
14 February 2019 – A group of private backers has stepped in to fund a national unit supporting courts which help parents deal with drug or alcohol addiction so their children are not taken into care.
The unit, which supports the 13 Family Drug and Alcohol Courts (FDACs), mostly in England, was forced to close last year when government funding was cut.
Since then, £280,000 has been pledged to fund a new national unit.
The aim is to expand the special courts to help more families stay together.
Supporters say this saves taxpayer money in the long run.
FDACs are led by specially trained judges and work closely with a team of social workers, psychiatrists and substance misuse workers.
Their day-to-day work was not affected by the closure of the national unit – but the unit was needed to set up new courts, co-ordinate the existing ones and train staff.
Research has found children are less likely to be taken permanently into care in cases heard in FDACs, and less likely to experience further neglect and abuse. Parents are also more likely to stop using drugs.
Professor Judith Harwin, from Lancaster University, welcomed the news and said that her team’s research on FDACs was ‘very positive.’
They found that 58% of the mothers who used an FDAC did not return to misusing drugs or alcohol, compared with 24% who went through ordinary court.
Mary Ryan, a former lawyer who was part of the original team that set up the system, said the courts designed to prevent parents coming back into the system over and over without their problems being sorted out and were ‘value for money’.
‘We believe this should be much more widely available to children and families across the country,’ she said.
Phil Bowen, director of the Centre for Justice Innovation, which will direct the new national unit, said the funding would help expand the valuable work of the courts.
‘They get to the root of difficulties faced by parents struggling with substance misuse using a therapeutic, problem-solving approach, giving vulnerable children a better start in life, keeping families together and saving taxpayer money,’ he said.
What are Family Drug and Alcohol Courts?
FDACs help families in which children are put at risk by parental substance misuse.
Most families seen by them have additional problems such as domestic abuse or parental mental health difficulties.
The court works with social workers, substance misuse specialists, psychiatrists and mentors to help parents keep their children.
Parents are given a “trial for change” that gives them the chance to overcome their problems with the support of professionals.
The same judge reviews the case every fortnight, usually without lawyers present.
The courts were modelled on US-style problem-solving courts. The first one was set up in London in 2008, with cross-government funding.
The Department of Education supported the rollout of FDACs, of which there are now 13 in England and Northern Ireland. However, last year it withdrew funding for the national unit which supports the courts, forcing it to close.
After the government stopped financing the national unit, a fundraising campaign was launched by the co-founders of Hall Brown Family Law Solicitors.
It followed a meeting with Judge Nicholas Crichton, who founded the first Family Drug and Alcohol Court in 2008, and the Earl of Listowel, who is one of the courts’ most prominent advocates in parliament.
The campaign was subsequently backed by LCM Wealth, which advises high net worth families; family law firm Family Law in Partnership; and AddCounsel, a provider of bespoke behavioural health programmes, along with other anonymous supporters.
Jonathan Ashworth: We can’t allow innocent children to suffer in silence
Shadow health sec leads line-up of guest speakers at annual NACOA event
14 February 2019 – ‘As an MP, I want to make sure other children don’t suffer in silence,’ said Jon Ashworth in an iNews article containing a moving testimony to his childhood years.
The shadow health secretary recounted the times living with his alcohol-dependent father in which the ‘fridge had no food, but was always fully stocked with cheap white wine’, and demanded we ‘must begin with tackling attitudes’ in order to tackle addiction.
This rallying cry came ahead of the annual National Association for Children of Alcoholics (NACOA) David Stafford Memorial Lecture, where the Labour Member of Parliament for Leicester South was one of a host of speakers who detailed their personal experiences with family members battling alcohol dependency.
Highlights of the event (see Alcohol Change UK tweet thread) included presentations from former England football team captain Tony Adams, Liam Byrne MP and television personality Calum Best. Daily Telegraph Associate Editor Camilla Tominey, who was also present at the event, said that NACOA would be featuring in an upcoming BBC Radio 4 documentary about children with alcohol dependent parents on 27 March.
In addition to the estimated 2.6 million children in the UK living with a parent who drinks too much alcohol (ie to a hazardous extent or is dependent), NACOA also says it also saw an increase in the number of requests for help it received last year, with more than 20,000 calls.
Despite these numbers, the issue is still largely invisible, with many children unwilling or unable to get the help they need, leading to issues that can persist long into their adult lives. The charity says children of alcoholics are six times as likely to witness domestic violence, three times as likely to consider suicide, and twice as likely to experience problems at school.
Speaking to Sky News, NACOA ambassador Josh Connolly said: ‘To young people who might be struggling with a parent who drinks too much we like to say “you are not alone in your struggles and you are justified in the way you feel”… and that help and support is there.’
Changing channels?
Video-on-demand content is a global driver of alcohol consumption
15 February 2019 – The exposure of young people to audio-visual tobacco and alcohol content is common on streaming services, forming a risk factor for smoking and alcohol uptake among young people, claims a new report, the first to explore alcohol and tobacco content in video-on-demand (VOD) programmes.
Previous UK research has quantified tobacco and alcohol content in films and broadcast television, but not that of video-on-demand (VOD) services such as Netflix and Amazon Prime. Researchers performed a content analysis of 50 episodes from the five most popular programmes provided by the streaming platforms in 2016, comparing findings with earlier studies of UK prime-time television content.
Of 2,704 intervals coded, alcohol content appeared in 363 (13%) intervals in 47 (94%) episodes. There were no significant differences between the two services, however the proportion of episodes containing alcohol was significantly higher in VOD original programmes than those recorded in an earlier study of prime-time UK television.

Alcohol branding seen in Netflix and Amazon Prime instant video original programming |
In conclusion, the researchers wrote: ‘Audio-visual tobacco and alcohol content is common in VOD original programmes and represents a further source of exposure to imagery causing smoking uptake and alcohol use in young people.
‘This appears to be equally true of services regulated in the UK and The Netherlands. Given that VOD services are consumed by a global audience, it appears likely that VOD content is an important global driver of tobacco and alcohol consumption.’
You can listen to lead author Dr Alex Barker speak about the paper in more detail on our Alcohol Alert podcast.
Welsh Government to press ahead with 50p minimum price
Adapted from Drink and Drugs News
18 February 2019 – The Welsh Government has committed to introducing a 50p minimum unit price for alcohol, following the results of a public consultation. ‘Ministers remain of the view that a 50p minimum unit price is a proportionate response to tackling the health risks of excessive alcohol consumption,’ the government announced.
The government will now ‘lay regulations’ to the National Assembly for Wales for consideration later this year, it states – the assembly has already supporting minimum pricing when the Public Health (Minimum Price for Alcohol) (Wales) Bill was passed last year.
There were almost 55,000 alcohol-related hospital admissions in Wales in 2017, as well as 540 deaths.
Minimum pricing came into force in Scotland last May following years of legal battles, while more than 100 MPs, health bodies and charities signed an open letter to the Sunday Times last year calling for it to be introduced in England ‘immediately’.
‘The Welsh Government has always said that minimum pricing forms part of a wider strategy and approach to reducing substance misuse,’ said Health Minister Vaughan Gething.
‘Following a public consultation, I’m pleased to confirm we will now ask the National Assembly for Wales to approve a 50p minimum unit price. We believe a 50p minimum unit price strikes a reasonable balance between the anticipated public health and social benefits and intervention in the market. We will continue to use all available levers to reduce the harms caused by the excessive consumption of alcohol, as we develop and take forward a new delivery plan for substance misuse.’
Many responses to the consultation supported the principle of minimum pricing, but also raised issues regarding the potential unintended consequences of introducing a minimum unit price for alcohol.
The minister added: ‘The consultation process raised a number of issues, such as the potential impacts on vulnerable groups, household budgets, the risk of switching to other substances and the potential increase in the number of people seeking support from services. We will continue to consider these potential impacts.
‘We have commissioned specific research to look at the risk of switching, which will report ahead of implementation. In December 2018, we announced an extra £2.4m in funding for Area Planning Boards for local frontline substance misuse services so that we can ensure services are widely available. We have worked closely with Area Planning Boards throughout the development of this legislation and we will continue to do so ahead of implementation.’
More late night levies for Londoners
Southwark and Redbridge both contemplating fee
Two London boroughs are looking to introduce late night levies (LNL) in their boroughs.
Southwark Borough Council is launching a 12-week consultation into the possibility of implementing a levy that would affect more than 400 businesses situated between London Bridge, Dulwich, Rotherhithe, Peckham and Camberwell.
A LNL is estimated to raise between £365,000 to £420,000 a year, which Southwark would want to use to tackle booze-related crime and anti-social behaviour across the borough, especially the ‘key crime hotspots’ of Borough High Street, London Bridge, and Elephant and Castle.
The London Borough of Redbridge has also launched a consultation which would affect businesses from Ilford to Chelmsford. Redbridge expects to make more than £115,000 from the levy.
The chair of the London Night Time Consultation, Kate Nicholls, has criticised the move, calling it ‘ridiculous’ and arguing that local partnerships were a better way of managing town centres at night than introducing the levy.
‘Such partnerships have been far better at bringing long-term benefits than imposing, for example, the Late Night Levy. We believe the levy should only ever be a last resort,’ Nicholls wrote in a report on London’s night time economy.
However a spokesperson for the council insisted that the levy would be targeted at dealing with the costs of policing the night time economy.
‘Police crime reports and complaints shows a clear correlation between the locations of late night licensed premises and incidents involving crime and disorder, including antisocial behaviour and public nuisance,’ the spokesperson said.
‘If the LNL is introduced, license holders has the right, if they so wish, to make an application to vary their licence. They can do this free of charge before it’s introduced so that the premises will not be subject to paying the levy,’ they added.
Glasgow’s alcohol court to deal with domestic abuse
Adapted from BBC News
19 February 2019 – Glasgow’s alcohol court is to be extended, a year on from its introduction.
Two sheriffs in the city currently deal with offenders convicted of offences where alcohol abuse was a significant contributory factor.
From next month, the court will also be able to deal with domestic abuse cases where alcohol played a role.
Sentencing aims to address alcohol-driven crime, with a focus on education and counselling.
Offenders can receive community sentences along with an order allowing the sheriff to monitor progress.
So far, offenders convicted of domestic abuse have not been admitted to the alcohol court, but a new programme offering an alternative to custody will allow the court to consider these types of offence.
Under the Caledonian System, now being rolled out in Glasgow, a convicted domestic abuser is enrolled on a programme which aims to address their violent behaviour and improve the lives of the women and children affected.
It is not an alternative to prosecution and if at any point the programme is breached by the perpetrator the case is returned to court for consideration of whether a separate sentence should be imposed.
Problem solving approach
The creation of the “problem-solving” alcohol court followed the success of the drug court, which was created in 2001.
Within six months of the pilot’s launch last year, the alcohol court was a permanent fixture.
It deals with offenders who plead guilty or who are convicted of public order or drink driving offences and charges involving violence or dishonesty, where alcohol abuse is considered to be a significant contributing factor.
Sheriffs in Glasgow can refer offenders to the court for sentencing.
Of the 128 referred in the last 12 months, 61% have been made the subject of an alcohol court order.
During the period, 51 community payback orders and 27 deferred sentences were imposed, with only three revoked for non-compliance.
Risk of alcohol harms rising among elderly
Adapted from IOGT-NTO
22 February 2019 – A new report from IOGT-NTO in collaboration with the Swedish Society of Medicine, The Centre for Education and Research on Addiction (CERA) at the University of Gothenburg, the Swedish Society of Nursing and the Foundation Ansvar för Framtiden shows that alcohol consumption and alcohol-related harms are increasing among older persons.
The report addresses the elderly’s increased sensitivity to the effects of alcohol which, in combination with the ageing process, may increase the risk of disease and accidents, even at relatively low consumption levels. It describes the relationship between alcohol and various diseases and problems from which the elderly may suffer, such as cardiovascular disease, diabetes, dementia, and cancer.
The report also highlights the significance of lifetime lifestyles for health in old age.
‘The older a person becomes, the higher the resulting blood alcohol content from the same amount of alcohol. This can explain why the risk of diseases and accidents rises even at relatively low levels of alcohol consumption’, says Sven Andréasson, professor of Social Medicine at Karolinska Institutet’s Department of Public Health Sciences.
‘It is important to draw attention to the health and social effects of alcohol on older people, that is, people over 65, because lifestyle factors amongst the elderly greatly affect the risk of morbidity’, Sven Andréasson continues.
The report’s authors comprise some of the world’s leading, international alcohol researchers. The researchers have collated and aggregated facts and figures from international studies in the field and evaluated the scientific strength of the results, and both describe the role of alcohol policy measures, and offer recommendations for guideline alcohol consumption levels for the elderly.
Harm indicators suggest that alcohol consumption is increasing amongst older persons in Europe. This creates new challenges for welfare systems.
‘Alcohol consumption by older persons is often unremarked on by the health and medical sector. It is our hope that this report can help increase awareness of this issue and that it both provokes interest and stimulates discussion. Both amongst medical and healthcare personnel and amongst other interested parties, not least the concerned age group’, says Johnny Mostacero, president of IOGT-NTO.
Is Heineken helping?
Sexual exploitation, underpaid workers, and supporting racist regimes: Dutch brewer’s business practices revealed in new book
28 February 2019 – Journalist Olivier van Beemen has released a critical case study about the business practices of Dutch brewing giant Heineken in Africa, involving accounts of promotional girls being intimidated on a large scale during their work, and enduring poor working conditions.
The revelations in the book have led to parliamentary questions being asked in both the Dutch national assembly and the European Parliament, a boycott in France, the divestment of a Dutch bank and the unilateral suspension of a partnership with a prominent NGO.
To get an idea of its content, read this long read in The Guardian.
The book has also been nominated for the Lira Scherpenzeel Prijs for ‘groundbreaking international journalism’.
Heineken in Africa. A Multinational Unleashed is available to purchase at Hurst Publishers.
ALCOHOL SNAPSHOT – Mapping the geography of alcohol harm
NHS Digital’s Statistics on Alcohol, England, 2019 is one of the major authoritative sources of data on alcohol consumption and harm in England. Amidst the wealth of data and graphics it contains is the chart below, which shows the rate of alcohol-related hospitalisations by local authority.

Alcohol-related hospital admissions per 100,000 people (broad measure) |
The areas shaded dark blue had the highest rates of hospital admissions, whereas those shaded grey had relatively lower rates. The chart identifies inner London, the North-East and North-West as hotspots for harm, with Salford suffering the most hospital admissions per 100,000 residents. By contrast, hospitalisations were lower across the South of England, with the lowest rate in Wokingham.
The data beneath the chart come from the Hospital Episode Statistics, the NHS database containing details of all hospital attendances in England. The chart displays the ‘broad measure’ for alcohol-related hospital admissions – this involves counting every instances where the primary reason for hospital admission or a secondary diagnosis were linked to alcohol, and weighting this by applying ‘alcohol-attributable fractions’, estimates of the proportion of cases of a condition that are due to alcohol.
Podcast
Our monthly podcast features interviews with experts from across the sector.
Government licensing reform sparks concerns over public health and local accountability
Professor Niamh Fitzgerald –
University of Stirling
Dr James Nicholls –
University of Stirling