In this month’s alert
Editorial – August 2017
Welcome to the August 2017 edition of Alcohol Alert, the Institute of Alcohol Studies newsletter, covering the latest updates on UK alcohol policy matters.
This month, low cost airline Ryanair leads calls for restrictions on drinking alcohol to be applied to flights. Other articles include: concerns rise over the marked increase in baby boomers’ drinking habits; alcohol brands are found to fail in their self-imposed duty to communicate UK drinking guidelines to consumers; and Irish Health Minister Simon Harris pledges to bring alcohol minimum pricing to the country in next parliament.
Please click on the article titles to read them. We hope you enjoy this edition.
TOP STORY: Airlines call for alcohol restrictions
BBC show ‘Plane Drunk’ highlights dangers of easily accessible alcohol
The Home Office says it is “considering” calls for tougher rules on alcohol, as results of a BBC Panorama investigation show that arrests of passengers suspected of being drunk at UK airports and on flights rose by 50% in the last year.
A total of 387 people were arrested in the twelve months to February 2017 – up from 255 people the previous year. Meanwhile, more than half of cabin crew who responded to a survey said they had witnessed disruptive drunken passenger behaviour at UK airports.
The arrest figures obtained by Panorama came from 18 out of the 20 police forces with a major airport in their area, chiming with findings from the Civil Aviation Authority, who reported that most of the 600% increase in disruptive passenger incidents in the UK between 2012 and 2016 involved the use of alcohol.
Trade body Airlines UK said it should be made illegal for people to drink their own alcohol on board a plane.
Survey
A total of 19,000 of the Unite union’s cabin crew members were surveyed and 4,000 responded, with one in five saying they had suffered physical abuse.
A former cabin crew manager with Virgin, Ally Murphy, who quit her job last October after 14 years, told Panorama: “People just see us as barmaids in the sky.
“They would touch your breasts, or they’d touch your bum or your legs. I’ve had hands going up my skirt before.”
Code of practice – a load of hot air?
In July 2016, the aviation industry introduced a voluntary code of conduct on disruptive passengers, which most of the major airlines and airports signed up to.
The code’s advice included asking retailers to warn passengers not to consume duty-free purchases on the plane, while staff were also asked not to sell alcohol to passengers who appeared drunk.
However, Panorama found more than a quarter of cabin crew surveyed were unaware of the code of practice and, of those who had heard of it, only 23% thought it was working.
One anonymous crew member told Panorama: “The code of conduct isn’t working… we’re seeing these incidents on a daily, a weekly, a monthly basis. It’s the alcohol mainly in the duty free that is the significant problem.”
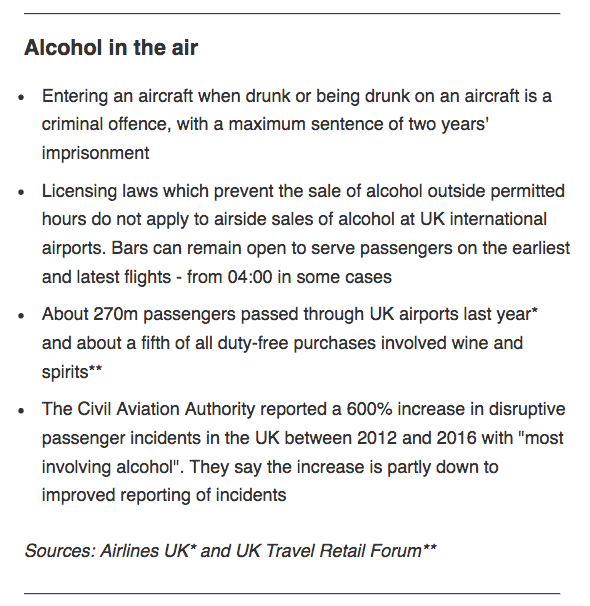
Current rules for passengers consuming alcohol while on board aircraft |
Alcohol in the air
Entering an aircraft when drunk or being drunk on an aircraft is a criminal offence, with a maximum sentence of two years’ imprisonment.
Licensing laws which prevent the sale of alcohol outside permitted hours do not apply to airside sales of alcohol at UK international airports. Bars can remain open to serve passengers on the earliest and latest flights – from 04:00 in some cases.
Manchester Airport is one of the signatories but when Panorama’s undercover reporter asked at World Duty Free whether she could open alcohol bought at a duty free shop to consume on the plane, she was told “officially probably not, unofficially I think you’ll get away with it”. Another shop in the airport did give the right advice.
World Duty Free said it was committed to dealing with the issue and that it displays “clear advisory notices at till points, on till receipts and on carrier bags that remind customers that alcohol purchases cannot be opened until their final destination is reached”.
Airlines UK, which represents carriers such as Virgin, British Airways and EasyJet, wants the government to amend the law to make consumption of a passenger’s own alcohol on board an aircraft a criminal offence.
Airlines call for action
In response to the documentary, Ryanair called for:
- a ban on the sale of all alcohol in bars and restaurants before 10am
- introducing the mandatory use of boarding cards when purchasing alcoholic drinks in bars and restaurants (in the same way a boarding card is needed for airport purchases) and limiting the number of drinks per boarding pass to a maximum of two
- controlling the sale of alcohol in bars and restaurants to passengers during delays by limiting the number of drinks per boarding pass to a maximum of two
Rival low-cost airline Jet2 has already banned alcohol sales on flights before 8am, and managing director Phil Ward agreed further action was needed.
“I think they [airports] could do more. I think the retailers could do more as well.
“Two litre steins of beer in bars, mixes and miniatures in duty free shops, which can only be there for one reason – you know, they’re items that are not sold on the high street.
“We can’t allow it not to change.”
The current Licensing Act (2003) does not apply to the sale of alcohol at airports. Earlier this year, a House of Lords committee report called for the rules to be toughened, concluding that “there is no justification for the Licensing Act not applying to sales airside at airports.”
Committee chair Baroness McIntosh of Pickering said: “We didn’t hear one shred of evidence to show the voluntary code was either working now or had any possible vestige of success in working any time soon.”
The Home Office said it was considering the report’s recommendations, which include revoking the airports’ exemption from the Licensing Act, “and will respond in due course”.
You can watch clips of the documentary by clicking through to the BBC Panorama Twitter page (via quote below):
Have you been on a flight like this? How do cabin crew feel about drunk passengers? More on @BBCPanorama pic.twitter.com/RbxgvKc3V8
— BBC News Press Team (@BBCNewsPR) August 14, 2017
Scotland: Alcohol-related deaths on the rise again
Annual totals at their highest level this decade (02 August)
New figures from National Records Scotland show that there were 1,265 alcohol-related deaths last year – an increase of 115 (10%) compared with 2015 – representing the highest annual total since 2010.
It was also the third largest annual increase in numbers since records began: there were increases of 151 (18%) in 1996 and 122 (11%) in 1999. The only other years with percentage increases of 10 or more compared to the previous year were 1988 (10%), 1994 (17%) and 1995 (12%).
There were 867 male deaths and 398 female deaths in 2016; the ratio of two male deaths to every female death related to alcohol has remained largely constant since 1979.
|
The cohort with the highest number of alcohol-related deaths in 2016 was aged between 45-59 (503 deaths), 12 more than in 2015 and the fourth consecutive increase. The 45-59 age-group has had the largest number of alcohol-related deaths in almost every year since 1979.
Older age cohorts seemed to suffer increases across the board. There was an increase of 56 in deaths of 60-74 year olds, to 468: a third consecutive increase, and the highest for that age-group since 2006. The 147 deaths of people aged 75 and over was 39 more than in 2015, and was the highest number ever recorded for that age-group.
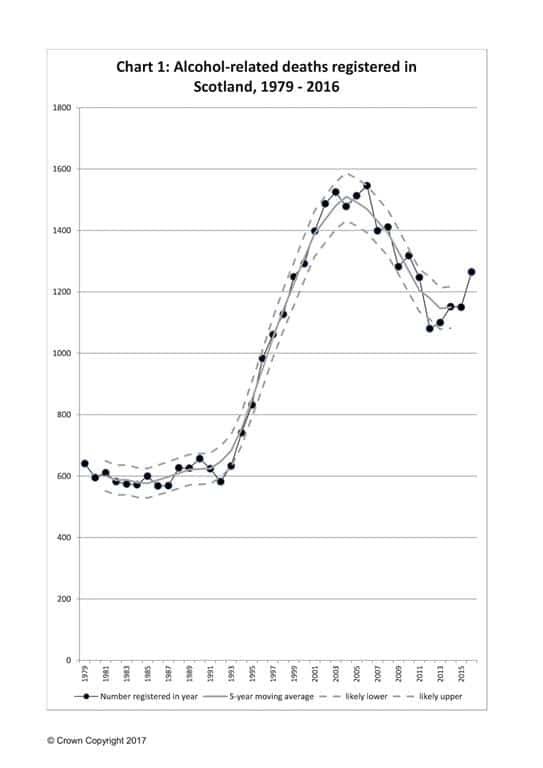
According to the National Records of Scotland website, the number of alcohol-related deaths was relatively stable, at roughly 600 per year, during the 1980s, before increasing rapidly during the 1990s and early 2000s, and reaching a peak of 1,546 in 2006.
Since then, the trend had appeared to be generally downward – reaching a recent low of 1,080 in 2012 – but remaining over 1,000 deaths. However, the report’s authors say that increases in three of the past four years, a larger increase in 2016 and an increase in the 5-year moving average may suggest a change in the direction of the trend (see chart, illustrated).
Commenting on the figures, Alcohol Focus Scotland chief executive Alison Douglas said:
“It is tragic that 1,265 men and women in Scotland died because of alcohol last year; a 10% increase on the previous year. Behind these appalling statistics are real people – sons, daughters, husbands, wives, parents, friends and colleagues – who have died too young because of a substance that’s cheap, widely available and constantly promoted.
“Alcohol-related deaths are preventable. Increasing the price of the cheapest, strongest drinks through minimum unit pricing will reduce consumption and save hundreds of people’s lives, particularly those living in our poorest communities. As well as minimum pricing, we need to see bold and proportionate action from the Scottish Government in its forthcoming alcohol strategy. This must focus on reducing the widespread availability and marketing of alcohol to make it easier for people to drink less.”
Seriously injured drink drive casualties rise
First increase in four years (04 August)
The number of people seriously injured in drink drive accidents is up almost 10% on the previous year, according to the latest statistics from the Department for Transport (DfT).
The final DfT estimates for 2015, ‘Reported road casualties in Great Britain: accidents involving illegal alcohol levels: 2015 (final)’ showed there were 1,170 serious injuries in reported drink drive accidents, up from 1,070 the previous year. Described by the DfT as “statistically significant”, this represents the first increase since 2011, and contrasts with the fall in the number of fatalities (from 240 to 200), as mortality figures stay at their lowest levels since records began.
Road safety groups called for stricter legislation to prevent the rise in serious injuries becoming a trend. Commenting on the new figures, Jason Wakeford, BRAKE’s campaign director, said: “Selfish drink drivers destroy lives and inflict appalling suffering on families up and down the country. There will be more, unrecorded, casualties involving drivers impaired by alcohol but under the current limit.
“The drink drive limit in England and Wales is the second highest in Europe and must be lowered urgently. In addition, savage cuts to road traffic policing must be reversed and enforcement increased to crack down on dangerous drink drivers.”
Kevin Clinton, head of road safety at The Royal Society for the Prevention of Accidents (RoSPA), said that the increase in the number of seriously injured shows “more action is needed, including reducing the drink drive limit, from 80mg (of alcohol per 100ml of blood) to 50mg, and ensuring the police are carrying out effective enforcement campaigns to deter people from having a drink before getting behind the wheel.”
The first set of provisional estimates to contain drink drive data for 2016 is scheduled for release at the end of September 2017.
Ireland: “Staggering” rise in young admitting drink driving
Proportion of young people drink driving double on previous year (07 August)
A survey of 1,000 respondents in Ireland has shown that people under the age of 24 are most likely to have driven a car after consuming alcohol.
Commissioned by Ireland’s Road Safety Authority, the research monitored attitudes in relation to alcohol and driving. The results of the survey carried out in January and February this year show:
- 73% of Irish motorists claim that having no alcohol before driving is the only way to be safe. However, 10% of Irish motorists have driven after consuming alcohol in the past 12 months, and of those who did, 23% claimed to have a ‘no alcohol’ limit before driving (illustrated).
- More than twice as many male motorists (14%) as female motorists (6%) have driven following the consumption of alcohol.
- 16% of those under 24 have admitted to drinking and driving in the past twelve months, up from 7% in 2015 and 4% in 2014, the biggest increases of any age group.
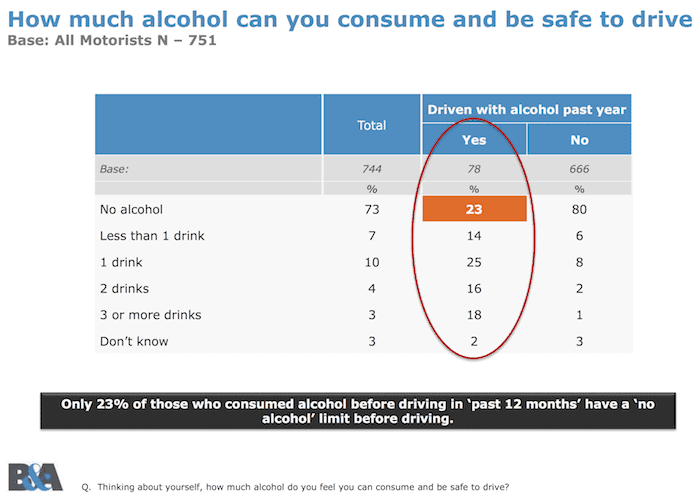
Only 23% of those who admitted drink driving thought it was unsafe to do so at all, compared with 80% of those who reported not drink driving |
The research also suggests that ‘high risk drivers’ especially those who admit to using a mobile phone while driving are twice as likely to have admitted to drink driving in the past 12 months.
Speaking to The Journal newspaper, RSA chief executive Moyagh Murdock said: “Our research shows there has been an increase in the number of young people having alcohol and getting behind the wheel of a car.
“We have done this survey for three years in a row and it has gone from 4% to 7% and alarmingly this year 16% of under 24s have admitted to taking alcohol and getting behind the wheel of a car.
“They are going to go out and kill themselves and kill other innocent road users,” said Murdock, who appealed to parents to sit down and talk to their young adult children about the risks.
“We are trying to get the messgae across to this age group and also to the parents of the under 24s – as some of them may be using the family car on the night out. Just because someone says they are driving tonight, it does not automatically mean that they are going to abstain from drink.
“As a society we have to be aware that people do take chances and we need to address it across the board, not just as individuals, but as friends and as family members, and to be alert to somebody who may be close to us engaging in that risky behaviour,” she said.
Garda chief superintendent Aidan Reid concurred, describing the 740 people a month (on average) arrested for being under the influence as a “staggering number”.
“The majority of people do listen and do take heed of the message and never ever drink and drive, but the young persons who are being detected for driving under the influence are just not listening,” he said.
Russian survey shows sobering results
Adapted from Tass Russian News Agency (14 August)
The number of Russians who do not consume alcohol has grown to 39% over the past eight years, according to the results of a survey conducted by the Russian Public Opinion Research Center.
“The results of the surveys show a decrease in the level of alcohol consumption in our country. While in 2009, 25% of Russians said they did not drink alcohol at all, in 2017 their number was 39% (47% among women and those aged between 18 and 24),” the pollster said.
On the other hand, 25% of those polled said they consume alcohol less often than once a month, and 16% of the respondents – two or three times a month. Just 5% of those polled said they drink alcohol every day of several times a week. Sociologists also registered a positive trend in terms of reducing alcohol consumption. About 44% of the respondents said they drink less alcohol than last year. At the same time, half of those polled (50%) said they consume the same volume of alcoholic beverages as a year ago.
According to the poll, most Russians (80%) believe that all alcoholic beverages have an adverse effect on one’s health, and there are no “harmless” alcoholic drinks. However, 15% of those polled still believe that some types of alcohol pose no threat to one’s health (citing primarily wine as an example).
The poll was conducted by the Russian Public Opinion Research Center on August 3-4, 2017, with 1,200 people aged over 18 interviewed, and was first reported by the TASS Russian News Agency.
Friday night (ambulance) on the town
Buzzfeed reporter tracks London paramedic on shift (18 August)
Alcohol-fuelled incidents slow down frontline services: This is the finding of Buzzfeed News reporter Patrick Smith, who was invited to witness a Friday night shift alongside a London Ambulance Service (LAS) paramedic.
Opening with the example of LAS paramedic Jake Carlson attending to a drunken person with minor injuries in Bethnal Green while another serious incident resulting in a life-threatening injury was unfolding five minutes’ drive away, Smith gave a glimpse of the strain that drunkenness puts on frontline NHS resources.
Although December is usually thought of as the busiest month of the year for attending alcohol-fuelled incidents (because of Christmas festivities), Smith found that the LAS will be called out to more alcohol-related incidents in this month (of August) than any other. “In 2016, the LAS dealt with 6,653 alcohol-related calls, 650 more than in December.”
Referring to the incident, Carlson told Buzzfeed that it’s the drunkenness that prevents him from moving to the other [more critical] incidents.
“This is the sad reality of it. OK, this guy has been assaulted and he has been injured and we’re here to help him – but he can’t be left alone because he’s been drinking… if you came out for this entire [12-hour shift] you’d see maybe two or three more of these.”
These revelations echo the findings of a report published by the Institute of Alcohol Studies in 2015 which found that half of ambulance staff surveyed reported having been injured on the job as a result of drunken violence. Emergency services are increasingly stretched, with over 90% of police and ambulance staff reporting they have performed the role of another blue light service in dealing with alcohol-related incidents, and over half of all emergency service staff said they feel inadequately trained to deal with alcohol-related incidents.
This August the LAS launched its first summer drinking campaign, #NotAnAmbulance, urging people to think twice before getting so drunk they can’t walk, to plan a route a home, and – crucially – to look after any friends on a night out who may have enthusiastically ignored this advice.
Adapted from Buzzfeed article ‘This is what it’s like to be a paramedic in London on a Friday night’.
Concerns over rise of substance misuse in “baby boomers”
Risky drinking among older people bucks consumption trends (23 August)
A rise in alcohol and drug misuse among the over 50s (commonly known as “baby boomers”) is causing concern, warn experts in The British Medical Journal (BMJ).
Researchers at South London and Maudsley NHS Foundation Trust and Flinders University in Australia say the number of people aged over 50 experiencing problems from substance misuse is growing rapidly, with the numbers receiving treatment expected to treble in the United States and double in Europe by 2020.
They call for a coordinated international approach to tackle this rapidly growing problem.
In both the UK and Australia, risky drinking is declining, except among people aged 50 years and older, they explain. There is also a strong upward trend for episodic heavy drinking in this age group.
But this generational trend is not restricted to alcohol, they add. In Australia, the largest percentage increase in drug misuse between 2013 and 2016 was among people aged 60 and over, with this age group mainly misusing prescription drugs.
However, people over 50 also have higher rates than younger age groups for both past year and lifetime illicit drug misuse (notably cannabis).
With alcohol being the most common substance of misuse among older people, under-detection of alcohol problems is of immediate concern – and may increase further as baby boomers get older because of their more liberal views towards, and higher use of, alcohol, they write.
A lack of sound alcohol screening to detect risky drinking may result in a greater need for treatment, longer duration of treatment, heavier use of ambulance services, and higher rates of hospital admission.
Research suggests that treatment programmes adapted for older people with substance misuse were associated with better outcomes than those aimed at all age groups.
However, the authors point out that clinicians will need improved knowledge and skills in assessing and treating older people at risk of substance misuse.
“There remains an urgent need for better drug treatments for older people with substance misuse, more widespread training, and above all a stronger evidence base for both prevention and treatment,” they write.
“The clinical complexity of older adults with substance misuse demands new solutions to a rapidly growing problem. So far, there has been little sign of a coordinated international approach to integrated care,” they conclude.
From ‘Substance misuse in older people’, BMJ. Link to full editorial here: http://press.psprings.co.uk/bmj/august/substancemisuse.pdf
Alcohol brands failing to communicate drinking guidelines
Time to move away from industry self-regulation of alcohol labels, new research shows (23 August)

AHA UK ‘Right to know’ report |
Hardly any alcohol brands provide accurate information about the low-risk alcohol consumption guidelines, 15 months after they were first introduced.
This is the revelation of a new Alcohol Health Alliance (AHA) UK report, ‘Right to Know: are alcohol labels giving consumers the information they need?’, which involved researchers examining the product labelling of alcohol brands’ beverages in supermarkets and off-licences across England, Wales and Scotland.
A total of 315 product labels across 27 locations were reviewed to check whether they included the following drinking guidelines, as recommended by the UK’s chief medical officers (CMO):
- Advice to stay within the low-risk weekly guideline of 14 units (for both men and women)
- Advice to spread out drinking across the week
- Health warnings of specific conditions like cancer, heart disease or liver disease
- Advice to have days without having a drink
- Advice that it is safest not to drink when pregnant or trying to become pregnant.
The results showed that only one label out of all 315 informed consumers of the low-risk weekly guideline of 14 units. More labels (seven) carried the Republic of Ireland guideline than the UK version.
Where products did refer to unit limits in the UK, the guidelines were out-of-date. Health warnings of specific illnesses or diseases – notably the increased risk of liver disease and cardiovascular disease from heavy drinking, and the increased risk of contracting at least seven different types of cancer from any level of drinking – were absent from the labelling too. No products adopted the CMOs’ advice to spread their drinking across the week, or have drink-free days. However, nearly all products included a pregnancy warning.
The AHA report concludes in its research that “alcohol industry self-regulation of labelling has failed, and that it is time for a regime of mandatory labelling of products to ensure they carry the UK guidelines and provide sufficient warning of the health harms linked with alcohol,” (see example below). This approach is supported by the public; AHA polling has found that 86% of people in the UK support mandatory product labelling for alcoholic beverages.
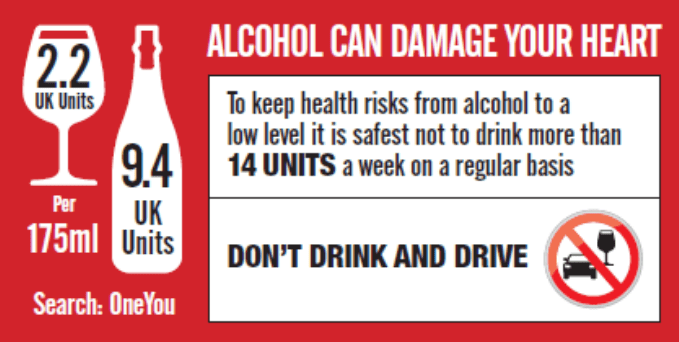
An alcohol label as imagined if supplied with accurate health warning information |
Commenting on the report, AHA chair Professor Sir Ian Gilmore said: “There is something seriously wrong with the system when consumers in the UK are more likely to buy a produce containing the Irish drinking guidelines rather than the current UK ones.
“Self-regulation has failed. Instead of alcohol producers deciding what to include on labels, the government should now require all labels to contain the latest guidelines and information on the health conditions linked with alcohol.
“Alcohol is linked with over 200 diseases and injury conditions, including cancer, heart disease and liver disease, yet awareness of these links is currently very low.We know, for example, that only 1 in 10 people are aware of the link between alcohol and cancer.
“The public have the right to know about the health impacts of alcohol, so that they are empowered to make informed choices about their drinking.”
Be mindful of your drinking
Just 11 minutes of mindfulness training can help heavy drinkers cut back (24 August)
Brief training in mindfulness strategies could help heavy drinkers start to cut back on alcohol consumption, finds a new UCL study.
After an 11-minute training session and encouragement to continue practising mindfulness – which involves focusing on what’s happening in the present moment – heavy drinkers drank less over the next week than people who were taught relaxation techniques, according to the study published in the International Journal of Neuropsychopharmacology.
“We found that a very brief, simple exercise in mindfulness can help drinkers cut back, and the benefits can be seen quite quickly,” said the study’s lead author, Dr Sunjeev Kamboj (UCL Clinical Psychopharmacology Unit).
The team invited 68 heavy drinkers to partake in the study – people that regularly drink more than the old weekly guideline limits (14 units a week for women, 21 units for men) and score ≥8 on the Alcohol Use DIsorders Identification Test.
Half of them were trained to practise mindfulness, which teaches a heightened awareness of one’s feelings and bodily sensations, so that they pay attention to cravings instead of suppressing them. They were told that by noticing bodily sensations, they could tolerate them as temporary events without needing to act on them. The training was delivered through audio recordings, and only took 11 minutes. At the end of the training participants were encouraged to continue practising the techniques for the next week.
The other half were taught relaxation strategies, chosen as a control condition that appeared to be just as credible as the mindfulness exercise for reducing alcohol use. The study was double-blind, meaning neither experimenters nor participants knew which strategy was being delivered.
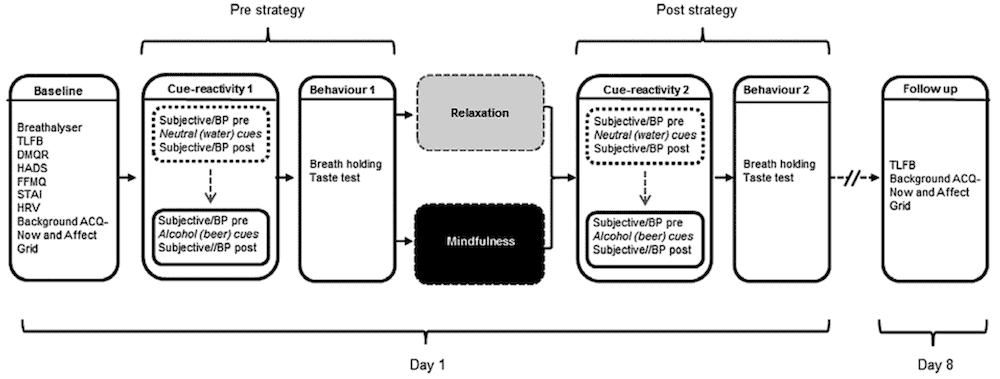
Experimental protocol for the within session (day 1) assessments and follow-up (day 8) procedures |
“We used a highly controlled experimental design, to ensure that any benefits of mindfulness training were not likely explained by people believing it was a better treatment,” said co-author Dr Tom Freeman (Senior fellow of the Society for the Study of Addiction), who was part of the research team while based at UCL.
The mindfulness group drank 9.3 fewer units of alcohol (roughly equivalent to three pints of beer) in the following week compared to the week preceding the study, while there was no significant reduction in alcohol consumption among those who had learned relaxation techniques (see illustration below).
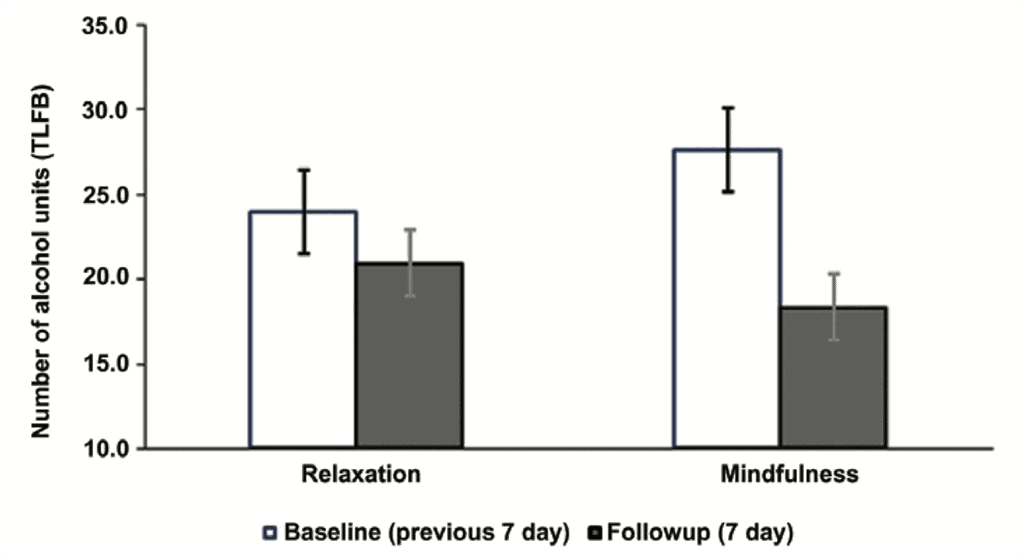
Average (mean) number of alcohol units consumed in previous seven days using timeline followback procedure |
Commenting on the findings, Liat Clark of WIRED UK wrote: “The success of the experiment, though small in scale, is impressive. It demonstrates that mindfulness could be used to instigate longterm health improvements. It provides an opportunity to break a habitual cycle, and show the individual that a relatively low-effort, simple technique can have a dramatic impact, potentially encouraging them to keep it up and replace one habit with another.”
The study’s authors explained that by being more aware of cravings, participants in the study were able to stop themselves from automatically reaching for a drink when they felt the urge.
“Practising mindfulness can make a person more aware of their tendency to respond reflexively to urges. By being more aware of their cravings, we think the study participants were able to bring intention back into the equation, instead of automatically reaching for the drink when they feel a craving,” Dr Kamboj said.
Severe alcohol problems are often preceded by patterns of heavy drinking, so the researchers are hopeful that mindfulness could help to reduce drinking before more severe problems develop.
“Some might think that mindfulness is something that takes a long time to learn properly, so we found it encouraging that limited training and limited encouragement could have a significant effect to reduce alcohol consumption,” said co-author Damla Irez (UCL Clinical, Educational and Health Psychology).
“It’s unclear, at this stage, whether the treatment would have the same impact on someone suffering from alcoholism, but it could potentially prevent a heavy drinker from becoming alcoholic,” WIRED’s Clark speculated.
The team are looking to follow-up this study with further experiments related to substance misuse: “We’re hopeful that further studies will replicate our findings and provide more insight into how mindfulness training could be most effective in practice. Our team is also looking into how mindfulness might help people with other substance use problems,” said co-author Shirley Serfaty (UCL Clinical, Educational and Health Psychology).
Substance misuse treatment funding down 16% since 2013
Removal of budget ring-fence may create “vicious cycle” for addicts (25 August)
Freedom of Information figures obtained by The Independent newspaper show that local councils across England have had to reduce spending on drug and alcohol support services by tens of millions of pounds since 2013, as death and ill-health linked to substance misuse hits record levels.
Experts say that the reduction in spending is creating a “vicious cycle” that is leaving the needs of serously vulnerable addicts unmet.
The 118 councils that responded to the FoI are spending a total of £452m on alcohol and drugs misuse strategies from public health grants this year, compared with £535m in 2013/14 – a cut of 15.5%.
Hospitals are seeing more than one million admissions relating to alcohol each year, with a review published by Public Health England late last year reporting that alcohol is now the “leading risk factor for ill-health, early mortality and disability” among 15 to 49-year-olds.
The new figures, obtained by leading addiction firm UK Addiction Treatment (UKAT), have fuelled growing concern over the Government’s decision to remove ring-fenced budgets for drug and alcohol treatment in 2012, which saw responsibility for public health passed onto local councils, equating to a real terms cut to local authority budgets.
The data shows that while 25% of public health grants were spent on drugs and alcohol strategies during 2013/14, this has fallen to 17% in the current financial year – indicating a projected real-terms cash cut of £105.1m in the services across all 152 unitary and upper tier councils in England.
The Local Government Association (LGA), which comprises local authorities in England and Wales, warned that while councils were committed to tackling substance misuse and providing drug users with adequate support and treatment, cuts to the public health grant were “seriously undermining” their efforts.
At the 2015 Spending Review, the Government announced a 3.9% real-terms cut in public health funding over the next five years, which drug and alcohol support services fear will exacerbate the country’s drug and alcohol dependency issues, placing further strain on the already stretched emergency services.
Eytan Alexander, Founder of UKAT, said the removal of the protected drug and alcohol treatment budget was a “catalyst for disaster” and has left councils having to “spin even more plates” but with access to smaller funds.
“What our Freedom of Information Requests reveal is that since the Government made the decision to remove the protected drug and alcohol treatment budget, councils have been forced into spinning even more plates with even less money,” Mr Alexander said.
“This decision was, without a doubt, a catalyst for disaster. Slashing budgets on substance misuse is a false economy as it simply piles the pressure on our already stretched emergency services. The alarming correlation between the real-term cut to Council budgets and the rise in drug-related deaths needs to be addressed and this vicious cycle needs to end.”
Paul Hayes, chief executive of Collective Voice, which represents the largest voluntary sector providers of drug and alcohol treatment in the UK, said providers were finding it increasingly difficult to meet the demand, and warned that the true cuts to funding are “even higher” than the FOI figures suggest.
“From our point of view, it’s gone down by even more than 15%, but it’s variable across the country. Our estimates are based on the changes in contract value between 2013, when there was protected funding, and now – which is about 25 to 30%. It’s incredibly difficult to get accurate numbers, but nobody disputes that there’s been a huge reduction in the amount available,” he said.
A Department of Health spokesperson said: “Local authorities are best placed to make choices about services for their community which is why decisions about public health spending sit with them. To help, we are giving them £16bn over the current spending period to deliver these services.
“Figures show drug abuse and alcohol consumption are falling, but we will not be complacent. We have shown that we are willing to take tough action to protect the public’s health – as the first country in Europe to legislate for standardised packaging of cigarettes, by introducing a comprehensive Drugs Strategy and in publishing a world-leading childhood obesity plan.”
Article adapted from The Independent.
Irish Health Minister: Minimum alcohol pricing on its way
Simon Harris says law could pass in next parliamentary session (28 August)
Legislation to introduce minimum pricing for alcohol could pass all stages of both Houses of the Oireachtas in the coming session, Minister for Health Simon Harris has said.
Speaking in Dublin at the launch of Recovery Month, an initiative being championed by the Rutland Centre for addiction treatment, Mr Harris called on all political parties and Independents to “step up to the plate” and support the Public Health (Alcohol) Bill.
As well as minimum unit pricing, the Bill includes provisions to regulate advertising and sponsorship of alcohol, to provide health labelling on products and to ensure structural separation of alcohol in shops.
Echoing the Rutland Centre’s own findings that alcohol was still the biggest addiction they were coming across, Harris said he had taken on board concerns raised in the Seanad (upper house) that the requirements would place an undue financial burden on small business owners and promised that he would reflect that in amendments to the legislation in October.
“I suggest we listen to medics and to clinical experts perhaps an awful lot more than we listen to some vested interests in this regard,” he said. “I believe you can make every ‘Trojan horse’ argument that you wish to dilute this legislation, but at the end of the day if we are serious about showing political leadership on alcohol, rather than political platitudes, we need to get on with delivering this legislation.”
Figures released on Monday from the Rutland Centre, which treats more than 400 people a year, show alcohol was the “number one drug of choice” in 91% of presentations there last year, up from 87% in 2015. The age of those people most frequently seeking treatment was between 34 and 44 years old.
Maebh Leahy, chief executive of the centre, also urged support for the legislation, as well as for the proposed Gambling Control Bill. She said one of the key messages of Recovery Month would be that “addiction can and does affect all types of families and communities”.
“If we can open up the conversation about addiction and let people know there is no judgment and that recovery is possible, then it may help more families who are currently living in situations from which they see no escape,” she said.
Recovery Month involves a series of free events throughout September looking at varied aspects of addiction recovery in specific communities.
ALCOHOL SNAPSHOT: Diageo’s Annual Report shows promise for the ‘Better, Not More’ strategy
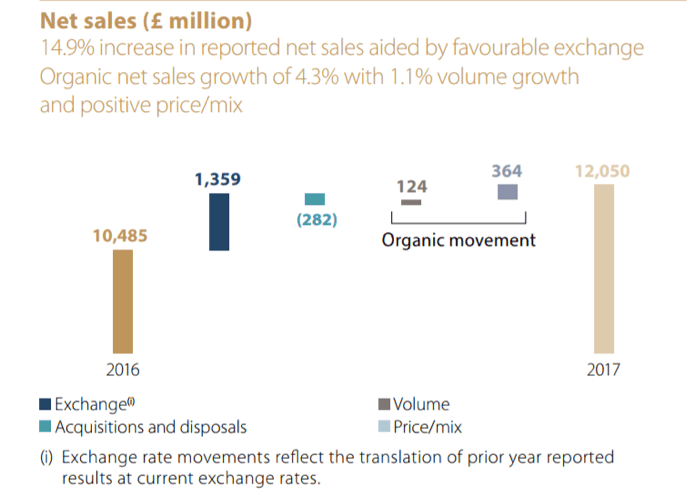
An ongoing debate with substantial relevance for alcohol policy is whether the alcohol industry can credibly claim to support lower levels of harmful consumption, given that this would seem to go against their commercial interests. A 2009 Health Select Committee concluded that it couldn’t, arguing that “the Government must be more sceptical about the industry’s claims that it is in favour of responsible drinking”. This, in turn, calls into question the viability of industry self-regulation (such as the Portman Group’s marketing code) and voluntary schemes such as the Public Health Responsibility Deal.
Alcohol industry groups, by contrast, insist that people drinking less does not necessarily mean people spending less. On this view, producers and retailers can make up for lower volume sales by increasing average prices – both through direct price increases and by encouraging consumers to ‘trade up’ to more expensive premium products.
The leading alcohol producer Diageo’s 2017 Annual Report, released earlier this month, makes exactly this argument: “Many consumers seek to drink ‘better, not more’ as they aim to develop their tastes while maintaining a balanced lifestyle, and are prepared to pay a premium for high-quality brands with heritage and provenance”.
The chart above, taken from the Annual Report, offers some support for the effectiveness of this strategy. It breaks down the various components of Diageo’s revenue growth between 2016 and 2017. First and foremost, it shows a huge ‘Brexit Bonus’: because the pound has weakened, the value of sales abroad in other currencies is higher, which is worth an extra £1.359 billion (a 13% increase) to Diageo.
However, more interesting is ‘organic growth’ in Diageo’s ‘core business’, stripping out these currency effects and purchases and sales of certain brands. This increased by £488 million over the year, of which £124 million was due to higher volume sales, and £364 million was due to higher average prices. In other words, price increases and premiumisation accounted for nearly three times as much of Diageo’s growth as higher volume sales.
Earlier this year, IAS carried out similar analysis for the UK alcohol industry as a whole, finding that between 2004 and 2014 premiumisation and price increases led to £6.3 billion of sales growth, but that this was offset by falling per capita consumption (which reduced sales by £4.3 billion) and the shift from the on-trade to the off-trade (which reduced sales by £3.8 billion).
Podcast
Our monthly podcast features interviews with experts from across the sector.
Bottling Up Trouble: alcohol, workplaces, and the need for change
Tabbin Almond –
Alcohol-freedom coach and author

