In this month’s alert
Editorial – August 2015
Welcome to the August edition of Alcohol Alert, the Institute of Alcohol Studies newsletter, covering the latest updates on UK alcohol policy matters.
In this issue, a new qualitative study questions whether the UK’s unit guidelines are relevant to people’s drinking habits. Other articles include: Middle-aged drinkers suffer worst from alcohol misuse in Wales; Study finds light to moderate drinking raises cancer risk; and regional report reveals the burden that alcohol places on ambulance staff in the North East.
Please click on the article titles to read them. We hope you enjoy this edition.
Study questions usefulness of current drinking guidelines
Researchers reveal gap between advised and actual drinking behaviours
The Government’s current alcohol guidelines are unrealistic and largely ignored because they have little relevance to people’s drinking habits, according to a new report by the University of Sheffield’s Alcohol Research Group (SARG) in collaboration with the University of Stirling.
The qualitative study – the first of its kind – explored how drinkers make sense of the current UK drinking guidelines, which suggest men should not regularly exceed three to four units of alcohol a day, while women should not regularly drink more than two to three units daily.
A team of researchers represented by the UK Centre for Tobacco and Alcohol Studies conducted focus groups to see how the current guidelines were perceived by people aged between 19- 65 years and from varied socioeconomic backgrounds. The results presented form part of a larger study, APISE (Alcohol Policy Interventions in Scotland and England), which aims to assess the impact and effectiveness of alcohol control policies in each country.
 The findings, published in the journal Addiction, show that the guidelines are generally disregarded as the daily intake suggestions are deemed irrelevant in a country where most people don’t drink everyday but may drink heavily at the weekend.
The findings, published in the journal Addiction, show that the guidelines are generally disregarded as the daily intake suggestions are deemed irrelevant in a country where most people don’t drink everyday but may drink heavily at the weekend.
The results also revealed that people think the recommended quantities of drink are unrealistic, as they don’t recognise that many people are motivated to drink to get drunk. Researchers found that participants preferred the current Australian and Canadian guidelines, which include separate advice for regular drinking and for single occasion drinking. These were regarded as more relevant and flexible to occasional drinkers.
Presenting the guidelines in units was also seen as a problem for many participants, who preferred to measure intake by the number of glasses, pints or bottles consumed instead. While unit measurements are useful for health professionals, they were seen as ‘too abstract’ for the general public. While participants did regulate their drinking, this was done in ways “which made more sense to their everyday lives”, wrote Melanie Lovatt from the University of Sheffield (pictured), who led the study. Long-term personal health stressed in the current guidelines – came second to avoiding more immediate negative consequences issues such as needing to go to work the next morning, having childcare responsibilities, or recovering from hangovers.
She said: “These findings not only help to explain why some drinkers disregard current guidelines, but also show that people make decisions about their drinking by considering their responsibilities and lifestyle, rather than just their health.”
When understood within the context of personal knowledge, experience and values, the report explains, the participants could be seen to act rationally. An alternative (but related) interpretation of the findings is that the apparent ‘failure’ of people to adhere to public health guidance may be explained by the ‘prevention paradox’: that while following the guidelines might result in the improvement of the nation’s health, many individuals may not see a noticeable improvement in their own health, “and therefore lack a sufficient incentive to comply with health guidelines”. Addressing the tension between public health concerns over alcohol and the perceptions and motivations of the general public is the central challenge for experts who are involved in updating the UK drinking guidelines.
Guidelines: Out with the old?
Alcohol misuse is estimated to cost the the NHS in England an estimated £3.5bn a year (at 2009–10 costs) and a further £400m in Scotland (2006/7 prices). This does not include any estimate for the economic costs of alcohol misuse to families and social networks. Guidance is needed to alert the public to the dangers of drinking to excess.
In its 2012 Alcohol Strategy, the UK Government announced a review of its lower drinking guidelines. The purpose of this was to take account of new evidence on the health consequences of drinking emerging since 1995 when the guidelines were last reviewed.
This report concludes that the insights of drinkers into how they monitor their consumption ought to be considered in the framing of a new set of guidelines. While the study did involve a small number of people (12 focus groups comprising between three to six participants; n total = 66), it does still pose a strong argument for taking culturally specific behaviour into account when forming public health guidelines.
Listen to Melanie Lovatt explain the report’s findings and its implications in more detail on our Soundcloud page: soundcloud.com/instalcstud
Report reveals burden alcohol places on North East ambulance staff
Almost half of North East paramedics have been assaulted by drunk patients or members of the public while on duty
Almost half of paramedics in the North East have been subjected to alcohol-fuelled threats and physical assaults whilst on duty, according to a new survey.
The Paying the Price report, published by Balance, the North East Alcohol Office, revealed that 2 in 5 paramedics surveyed have been subjected to alcohol-fuelled sexual assaults or harassment during their work.
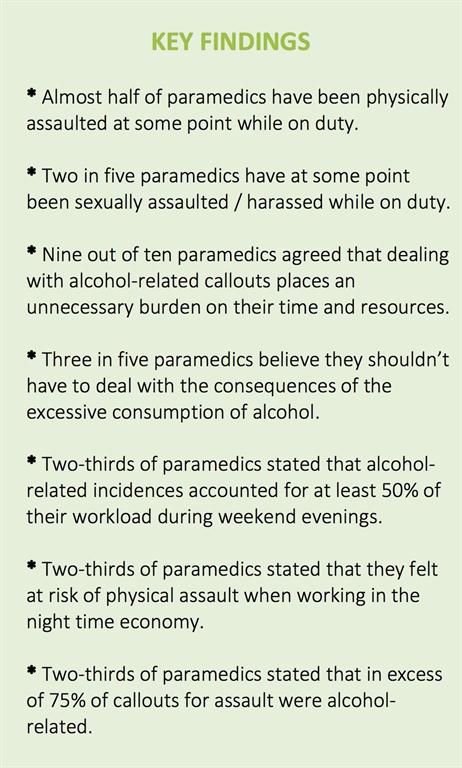
Unsurprisingly, they’ve had enough, says Balance, with 3 in 5 survey respondents saying that they shouldn’t have to deal with the consequences of alcohol misuse.
Alcohol misuse in the North East puts a huge financial strain on the region’s frontline services. Balance estimated that alcohol misuse cost the region around £911 million in 2013/14, including a cost to the NHS of £242 million.
The alcohol charity partnered with the North East Ambulance Service (NEAS) to carry out a survey of 358 paramedics between April and December 2014, representing 32% of the NEAS workforce (key findings illustrated).
The stories of harassment and abuse by drunk patients towards staff were especially common. An experienced female paramedic who took part in the survey said: “I’m regularly sworn at by patients, their friends or relatives. The fear of being assaulted or sustaining injuries is increased when dealing with intoxicated patients.”
A fellow colleague who also shared her experiences of dealing with drunk patients. She said: “The sexual harassment from males can get out of hand. I tend to ignore this so to not start any conflict but many a time I do say to stop or I’ll get the police. Sometimes the threat of police can calm them but most of the time the threat or their presence can make things worse.”
Reflecting on the survey results, Yvonne Ormston, NEAS Chief Executive, said: “Our crews don’t just deal with drunk weekend revellers; our crews see the effects of alcohol at all times of the day and all times of the week, spread across our region and from patients of all ages and backgrounds.
“For our staff, this is more than a job. But alcohol related calls take up far too much of our time and are often an abuse of our service, taking our resources away from patients who need us most.
“Intoxicated patients take much longer to triage on the phone and are more likely to be aggressive, placing staff in potential danger and increasing their stress levels.
“We take a zero tolerance approach to assault and support staff every step of the way if they have been abused. All staff also have access to a counselling service and a number of helplines to ensure their mental health is looked after as much as possible.
“We are pleased to be working with Balance to highlight the issues we face.”
Balance calls for a range of targeted, evidence-based measures – such as increasing the price of the cheapest, strongest alcohol products – to make alcohol less affordable, available and less widely promoted.
Colin Shevills, Director of Balance, said: “It’s outrageous that paramedics don’t feel safe in their working environment as a result of other people’s alcohol misuse. These are people who are there to help us when we need it most, yet they are living in fear of physical and verbal abuse on a daily basis. How many of us would expect to work like this?
“It’s clear from this report that our paramedics are personally paying the price for the alcohol misuse of others. This is an unnecessary burden on time and resource and it is completely unsustainable.
“Our relationship with alcohol is out of control. We need to bring it under control by making alcohol less affordable, available and less widely promoted. We need the Government to support a range of targeted, evidence-based measures such as increasing the price of the cheapest, strongest alcohol products, which has been shown to save lives, reduce hospital admissions, cut crime and lessen the financial burden alcohol places on frontline services.”
The relationship between alcohol and gambling behaviours
Report investigates a possible correlation between drinking and gambling problems
Alcohol Concern Cymru has published a new report “Alcohol and gambling research – The Relationship Between Alcohol and Gambling Behaviours”, in collaboration with the University of Roehampton Business School, which reviews the existing evidence on drinking and gambling.
The findings from the study shine a light on the relationship between drinking and gambling problems, with the authors concluding that more research is needed in this area in order to establish definitively whether there is a correlation and whether it is causal.
The report breaks the gambling concept into four key areas: 1) betting shops; 2) bingo halls; 3) casinos; and 4) online gambling. When looking at the links between gambling and alcohol consumption, the areas of greatest concern are identified in the report as the betting shops and online gambling.
The study identifies health survey prevalence data as having shown that participation in gambling is higher amongst more frequent drinkers, and that those who engage in multiple forms of gambling are more likely to consume more units of alcohol on their heaviest drinking day. However, these data do not indicate whether the drinking and gambling are taking place at the same time.
Whilst there is more research on comorbidity and problem gambling, there is relatively little research on ‘normal’ gambling behaviour in different sectors and the extent to which and way in which it is combined with alcohol consumption. Destination gambling venues such as land-based casinos and bingo halls are environments where it is possible to observe and, to some extent, to control how drinking and gambling are combined. Operators are required by the regulators to prevent customers who are drunk from gambling. However, there is little research looking at gambling and drinking behaviour in these venues.
By contrast, in the two sectors of the industry which are of current concern to the regulator – machine gambling in betting shops and online gambling – it is much harder to observe behaviour. In the former case, the drinking (if it is happening) would be happening at a different venue and in the latter case, because the gambling can be easily hidden (and the drinking as well if both are happening at home). In both these cases there is again little research, although some studies suggest that drinking and online gambling are commonly combined.
International research has identified a consistent theme of alcohol use contributing significantly to impaired control of gambling, and there is a relationship between gambling and binge drinking. Research has also shown that there is a tendency to drink in response to ‘wins’.
Environmental, social and cultural factors significantly influence gambling and alcohol consumption. Other research has shown that the extensive use of alcohol and drugs is a significant factor and risk predictor linked to problematic gambling.
The report further analyses the consumers of both alcohol and gambling activities, and the literature shows that individuals who are facing problems with gambling also are more likely to have other addictive behaviours, e.g. alcohol and/or drugs. For instance, research undertaken with university students found that students who drink to cope and have other indicators of alcohol problems also gamble to cope, gamble to win and have higher involvement and gambling related problems. However, the literature also shows that the processes underlying this association are not well understood.
Another important finding in the report is that at present, national substance misuse strategies in the UK do not incorporate behavioural addictions such as gambling. This is yet another reason for the further exploration of the relationship between alcohol and gambling problems, which is still in its infancy.
When considering treatments for gambling disorders, whilst the mainstay treatment is currently based on psychosocial interventions and pharmacotherapy for co-morbid conditions, the report discovered that there was an increasing understanding of the overlap of genetics and brain mechanisms involved in Alcohol Use Disorders and gambling. This implies that the treatments used in alcohol may be transferable in principle to gambling disorders.
Dr Guy Bohane, lead researcher for the study, explained:
“Health survey prevalence data have identified that participation in gambling is higher amongst frequent drinkers, and those who engage in multiple forms of gambling are more likely to consume more units of alcohol on their heaviest drinking days. However, there are clear gaps in the research. For example, the data doesn’t show whether this drinking and gambling is taking place at the same time.
“Similarly, we know that both drinking at home and online gambling, which often takes place behind closed doors, have grown considerably in recent years, yet there are few studies that have examined how these behaviours might be combined. There is also a lack of research into how different forms of marketing impact on those who drink and gamble at the same time, especially for young adults.”
Alcohol’s harm to others: new British studies in a wider perspective
 Guest article by Robin Room and Georgia Rankin
Guest article by Robin Room and Georgia Rankin
For many years, in thinking about problems from drinking the primary consideration was the problems for the drinker. The public health interest was defined primarily in terms of the effects on the drinker’s health and life circumstances, and in terms of providing treatment for drinkers who had become alcoholics. Only in limited circumstances, notably for drink-driving, was there clear recognition that many of the problems from drinking are problems for others around the drinker.
In the last few years, thinking has begun to change, with a wider recognition of the problems that drinking can pose for others – for anyone from someone who has drunk a lot in the street or other public places, and also notably for those close to and interacting regularly with the drinker, such as the drinker’s partner, children, other relatives, friends and work colleagues. The earliest fully-rounded study of these problems, as experienced by the others who had been adversely affected by the drinking, was conducted in Australia in 2008.
Now the idea of such studies has spread widely. Results are currently being compiled from a World Health Organization study of alcohol’s harm to others in seven low-and middle-income countries. Meanwhile, sets of questions about harms from others’ drinking have been asked in population surveys in several countries with levels of alcohol consumption and drinking customs like Australia’s. The questions asked are often drawn from or close to the questions on the Australian survey, allowing comparisons.
A recent report by the UK Institute of Alcohol Studies gives the results of such surveys in Scotland and North West England (the part of England stretching up the west coast from Chester to the Scottish border, and including Manchester and Liverpool). While these two surveys were of the general population, they were not necessarily representative – in particular, the North West England respondents were drawn from volunteers to answer market research surveys. Still, it is interesting to compare the rates of reported harms from drinking within the last 12 months on the British surveys, and on similar survey questions in New Zealand and Ireland, with the rates that Australians reported (illustrated below).
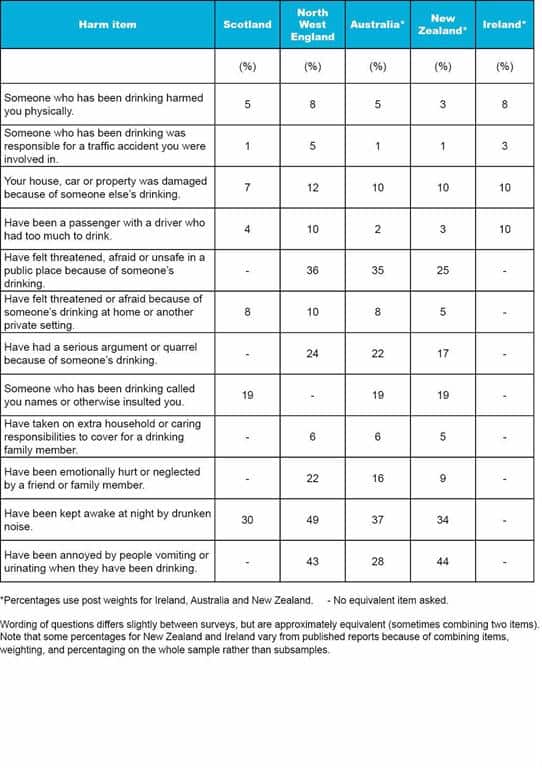 The profile reported across rates of different harms looked somewhat similar in the five societies. Quite serious tangible harms such as being physically harmed by someone who had been drinking, or having one’s property damaged because of someone else’s drinking, were reported in all five societies, though only a minority of the population had experienced such a harm in the past 12 months.
The profile reported across rates of different harms looked somewhat similar in the five societies. Quite serious tangible harms such as being physically harmed by someone who had been drinking, or having one’s property damaged because of someone else’s drinking, were reported in all five societies, though only a minority of the population had experienced such a harm in the past 12 months.
At an intermediate level, with rates ranging from about 1 in 6 to 1 in 3, were the reported rates of negative effects that would have been disturbing to experience, and which could have more lasting effects on quality of life – such as having a serious argument or quarrel because of someone’s drinking, feeling threatened, afraid or unsafe in a public place, because of someone’s drinking, or feeling emotionally hurt or neglected by a friend or family member. The most commonly reported – by one-quarter to one-half of respondents – were adverse effects which adversely affect community amenity: being annoyed by drinkers vomiting or urinating in public places, or being kept awake at night by drunken noise.
The general pattern across all five societies, then, is that adverse effects of drinking on the community’s general liveability are very widely experienced. Effects of others’ drinking which are threatening or emotionally upsetting are also quite widely experienced in the population. More serious tangible harms from drinking are less common, but regularly occur in all five of the societies.
Reported rates of experiencing the harms are often a little lower in New Zealand than elsewhere. They were generally higher in North West England, though this might in part reflect that the sample there may be less representative of the population. Rates in Australia tend to fall in about the middle of the range in these five societies with rather similar drinking cultures.
Any way of looking at it, in these societies where drinking alcohol is a regular part of the life of a majority of the adults, and where heavy drinking on weekends or special occasions has wide social acceptance, the harms from others’ drinking are both substantial and widely spread.
Article originally posted on DrinkTank website: http://drinktank.org.au/2015/08/alcohols-harm-to-others-new-british-studies-in-a-wider-perspective/
Recovery Partnership Review of Alcohol Treatment Services in England: Final report released
Review highlights key issues and themes facing the sector
 The report “The Recovery Partnership Review of Alcohol Treatment Services” (Mike Ward, Mark Holmes and Lauren Booker) is a review of the current state of alcohol treatment in England. Funded by the Department of Health and undertaken by Alcohol Concern on behalf of the Recovery Partnership, the report reflects the work from a six month project assessing how recent changes in health and social care have impacted on (i) the user journey through services, (ii) commissioning of services, (iii) training of staff and (iv) needs for specific groups.
The report “The Recovery Partnership Review of Alcohol Treatment Services” (Mike Ward, Mark Holmes and Lauren Booker) is a review of the current state of alcohol treatment in England. Funded by the Department of Health and undertaken by Alcohol Concern on behalf of the Recovery Partnership, the report reflects the work from a six month project assessing how recent changes in health and social care have impacted on (i) the user journey through services, (ii) commissioning of services, (iii) training of staff and (iv) needs for specific groups.
The report is based on online surveys, stakeholder workshops and interviews with services providers, commissioners, users, carers and with people working in other services linked to the alcohol treatment services. The project team conducted three online national surveys, interviewed 46 people and ran 14 workshops, representing a mixture of commissioners, service providers, service users and non-specialist staff.
The report does not make recommendations, but rather aims to identify key issues and inform the continued debate about alcohol treatment in England.
The report points out that there have been great changes to the alcohol treatment system over the last three years with two-thirds of respondents saying local services had been recommissioned during the period. 40% of respondents answered that, despite such upheavals, services had improved in that time. One clear change identified in the report is the merging of the drug and alcohol services, which led to access to more resources combined and an integrated system for treatment. Another important finding is the recognition of alcohol-related problems in the system.
However, the report still identifies challenges in the system, and gives attention to several issues, most notably: (i) the tender process; (ii) the division of mental health and alcohol problems; (iii) inadequate support for carers; and (iv) the need for further professional training.
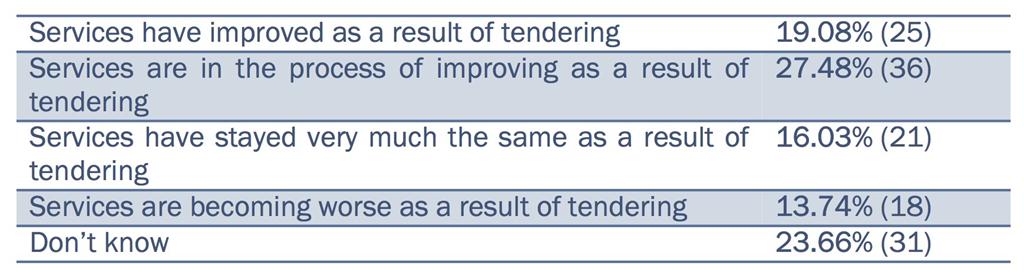
The tender process: The tender process is identified as a potential problem, with concerns raised that user needs are not necessarily prioritised. 68% of respondents said that services had been re-tendered in the past three years, and the report points out the uncertainty for both staff and services that this creates, which potentially jeopardises the quality of services when contracts are short term. However, only 14% of respondents felt that services had worsened at a result of tendering, while 47% believed that services were either in the process of or had improved as a result of tendering (illustrated).
 Dual diagnosis: The clearest message from the report was that there was a challenge to meeting the needs of more complex service users. 55% of respondents answered “No” to the question “Are there appropriate care pathways for people with both mental health and alcohol problems?”. Today, different bodies commission the services for mental health (CCGs) and alcohol (Public Health) areas. The report claims that the needs of the dually diagnosed have not been met, and points out the issue of separation between the two services as a reason for this.
Dual diagnosis: The clearest message from the report was that there was a challenge to meeting the needs of more complex service users. 55% of respondents answered “No” to the question “Are there appropriate care pathways for people with both mental health and alcohol problems?”. Today, different bodies commission the services for mental health (CCGs) and alcohol (Public Health) areas. The report claims that the needs of the dually diagnosed have not been met, and points out the issue of separation between the two services as a reason for this.
Support for carers: Another finding involves the lack of support for carers and concerned others, which is a group that receives too little help in the current system according to the respondents. The majority of carers seeking help are female partners, followed by parents. Since the group of carers and concerned others is very diverse and hard to reach, there are few clear recommendations for what is needed for this group.
Professional training: The report shows that training of non-specialist staff has been strengthened, particularly training in alcohol Identification and Brief Advice (IBA). Despite these efforts, respondents called for further improvements, including the introduction of a system of professional accreditation. This was followed by comments that medical staff who engaged in the training were being replaced with the non-specialist workers. This point was also raised in the context of tendering, where contracts would have a short term character and be less attractive than permanent positions in other services.
The report concludes by pointing out the need for a greater level of national guidance over alcohol treatment services. Its authors acknowledged that it will be hard (even more so separately) to find solutions to themes identified in the report, such as the frequency of tendering, the needs of the dually diagnosed, professional training structures and the investment in IBA.
Government reviews effect of alcohol addiction on employment
Adapted from Alcohol Policy UK
A review into the effects of drug and alcohol dependency on employment outcomes has been released by the Department for Work and Pensions (DWP). Led by Dame Carol Black, the document includes a ‘call for evidence’ into treatments or programmes that work, and experiences of service providers and users.
It says 1 in 15 working age benefit claimants are ‘suffering from alcohol dependency’; around 170,000 people. According to Government figures released last year, 53,880 claimants of Employment and Support Allowance (ESA), Incapacity Benefit (IB), or Severe Disablement Allowance (SDA) did so with a primary disabling condition of alcohol misuse in 2013, representing 2.2% of all claimants.
Drug Recovery Pilots, as set out in the Welfare Reform Act 2009, had planned to provide extra support for those voluntarily disclosing a drug or alcohol problem, as well as the power to test and impose conditions. However the DWP soon said ministers had decided not to take it forward and promised a radical ‘re-think’.
Yet with welfare reform integral to the Conservative Government’s ambitions, it comes as no surprise that claimants with substance problems are coming under renewed attention. Last year the Government announced that it would introduce pre-paid benefit cards to prevent spending on alcohol, drugs or gambling, whilst the Conservative election manifesto (2015) declared alcohol dependency as one of the the ‘root causes of poverty’. David Cameron also announced that he had asked Dame Black “to consider whether people should face the threat of a reduction in benefits if they refuse to engage with a recommended treatment plan”.
An opinion piece published in the Guardian criticised linking benefits to treatment as “unethical, and probably illegal”, stating that “the evidence suggests that, in general, positive incentives encourage positive behaviours and negative ones don’t.
“Far from reducing costs and freeing up resources (a perfectly legitimate goal) this is much more likely to waste resources by forcing people into treatments that they don’t want.”
A blog by the Centre for Economic and Social Inclusion also responded with an exploration of the some of the implications. The authors suggested improving the provision of treatment services by “reintroducing dedicated co-ordinators, improving co-location and outreach by Jobcentre Plus, and delivering on more joined-up – and supportive – casework”.
With Drugscope no longer in existence, it will be left to Alcohol Concern and others in the treatment field to highlight service provider perspectives. Certainly recent findings from the Recovery Partnership around the challenges in supporting dual diagnosis and complex needs are likely to bear relevance.
New national alcohol and drug strategies are likely to appear next year. The consultation closes on 11 September 2015.
Drink-driving deaths remain at low levels
Drink-driving now accounts for 14% of all fatalities on British roads
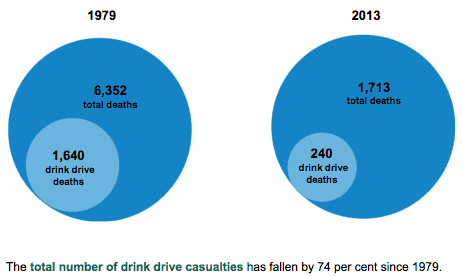
Final estimates for reported road accidents involving illegal alcohol levels in Great Britain show that in 2013, between 220 and 260 people (central estimate 240) were killed in accidents where at least one driver was over the drink drive limit. Drink-drive deaths now account for around 14% of all road fatalities.
Department for Transport figures also confirm that there were an estimated 230 fatal drink-drive accidents in 2013, an increase of 9.5% (20) on 2012 (210), and the highest number of fatal drink-drive accidents since 2009.
In contrast, the total number of drink-drive accidents of all severities fell by 14% to 5,690 in 2013. This means that around 4% of all reported road traffic accidents in 2013 involved at least one driver over the drink limit (illustrated). It is also the lowest number of drink-drive accidents on record.
However, because fatal casualty totals are subject to “considerable uncertainty”, they should be regarded as having unchanged since 2010, according to the DfT.
Long term trend data show that the number of fatalities from drink-drive accidents are more than six times lower today than in 1979, when records began. The total number of drink-drive casualties has since fallen by 74%.
A DfT spokesman said: “Tackling drink-driving is a priority for this Government and we have strengthened enforcement by removing the automatic right for drivers who fail a breathalyser test to demand a blood or urine test. This has denied people the chance to sober up while waiting for the test to be taken.
“High-risk offenders are now also required to prove they are no longer alcohol-dependent before being allowed to drive.
“The Government will be looking at the best ways to improve road safety during this Parliament and beyond.”
‘Report road casualties in Great Britain: Estimates for accidents involving illegal alcohol levels: 2013 (final) and 2014 (provisional)’ is a Department for Transport release which presents estimates of casualties arising from reported accidents involving at least one motor vehicle driver or rider over the legal alcohol limit for driving, in Great Britain in 2013 and 2014. Figures are derived from the Stats19 forms completed by the police plus toxicology data for road fatalities from coroners and procurators fiscal.
Wales: Middle-aged suffer worst from alcohol misuse
Increases in referrals for alcohol treatment across the board for those aged over 30, according to new substance misuse dataset
More than half of people (54%) referred for help with substance misuse in Wales have alcohol problems, prompting calls for minimum pricing.
In 2013/14, nearly 13,500 of the 24,806 referrals were because of alcohol, according to new government figures. Both figures are up on the previous year, although as a percentage of the total number of referrals, the proportion of people referred for help who have alcohol problems remains the same.
The figures show the biggest age group for alcohol problems is those aged between 30 and 49. Trend data (illustrated below) demonstrate that this has been the case as far back as 2009-10, although the largest increase in referrals on the previous year occurred in the oldest age group (60+).

“Part of the answer for me is around the pricing strategy,” said Clive Wolfendale, chief executive of drug and alcohol charity Cais. Mr Wolfendale acknowledged the Welsh government is planning to introduce minimum 50p per unit pricing but accepted there were European law “issues” around it along with the power drinks companies have.
He said: “It’s long overdue and there’s a huge weight of evidence that it can have an impact. People are stopping smoking because there’s clear recognition of the health risks and because they [cigarettes] have become so expensive.
“Some clients say they don’t care how much it [alcohol] costs, they will get it. Someone with a long term problem will beg and steal.
“But we can dissuade the student binge drinkers of today from turning into tomorrow’s addicts with higher prices and health education.”
Even light drinking raises cancer risk
Limit alcohol to one drink a day for women and two drinks a day for men, say experts
Even light and moderate drinking (up to one drink a day for women and up to two drinks a day for men) is associated with an increased risk of certain alcohol-related cancers in women and male smokers, suggests a large study published in the British Medical Journal.
Using data from two large United States studies, a team of researchers from Harvard University and Brigham & Women’s Hospital in Boston tracked the health of 88,084 women and 47,881 men for up to 30 years. They assessed risk of all cancers as well as known alcohol-related cancers including cancer of the the colorectum, female breast, liver, oral cavity, pharynx, larynx and esophagus.
The researchers used US measures of alcohol, which do not convert directly into UK units. They defined light to moderate drinking as less than 15g of alcohol for women and less than 30g of alcohol for men. One UK unit includes 8g of alcohol – for women, 15g of alcohol is just over 2 units. For men, 30g of alcohol is just under 4 units.
During the follow-up period, a total of 19,269 and 7,571 cancers were diagnosed in women and men, respectively. The results showed that light to moderate drinking was associated with a small but non-significant increased risk of total cancer in both men and women. But among women in particular, even consuming a single alcoholic beverage on a daily basis raised the increased risk of alcohol-related cancers, especially breast cancer.
The risk of alcohol-related cancers was also higher among light and moderate drinking men who had smoked at least once in their lifetimes, especially colorectal cancer. No association was found in men who had never smoked.
In an accompanying editorial, Dr Jürgen Rehm (Centre for Addiction and Mental Health in Toronto) said more research is needed to explore the interaction between smoking and drinking on risk of cancer, but, advised that roughly speaking, women should not exceed one standard drink a day (UK: 2-3 units) and men should not exceed two standard drinks a day (UK: 3-4 units).
He added that people with a family history of cancer “should consider reducing their intake to below recommended limits or even abstaining altogether, given the now well established link between moderate drinking and alcohol-related cancers.”
This sentiment was echoed by Dr Richard Roope, clinical lead for cancer at the Royal College of GPs. “We have known about the strong link between alcohol and cancer for some time, but this study serves as a useful reminder about how pronounced this is, especially when coupled with smoking, and when people have a family history of cancer,” he said.
Scotland: Alcohol-related deaths up 5% on last year
Alcohol misuse kills 20 Scots a week
Statistics published by the National Records of Scotland (NRS) show that there were 1,152 alcohol-related deaths in 2014, roughly 20 deaths a week on average.
This represented a second consecutive rise since 2012 and a 5% increase (52) on the previous year (1,100 in 2013).
More than twice as many men as women died of alcohol-related causes (784 male, 386 female).
The largest number of alcohol-related deaths was in the 45-59 age group (482), 10 more deaths than in 2013. The 45-59 age-group has had the largest number of alcohol-related deaths in almost every year since 1979.
The largest increase in deaths occurred among people aged 75 and over. There was a 24% increase − 23 more deaths − on the previous year to 118 alcohol-deaths in 2014, the highest number of alcohol-related deaths since records began.
The figures have prompted calls from public health professionals to speed up the introduction of minimum unit pricing in order to curb the widespread availability of cheap alcohol in Scotland.
Scottish public health minister Maureen Watt said: “This increase in alcohol-related deaths is disappointing, particularly given the decreasing trend we have seen in recent years.
“Alcohol deaths in Scotland are almost double those in the early 1990s. The 5% increase in 2014, following a 2% rise the previous year, shows that even though significant progress has been made since 2006 far more needs to be done.
“There is no doubt that a key factor in alcohol-related harm is affordability. This is why minimum unit pricing is such an important part of our package of measures to tackle the availability of cheap, high strength alcohol that causes so much damage in our communities.”
BMA Scotland Chair Dr Peter Bennie said: “It is disappointing to see the rise in the number of alcohol-related deaths, but it does underline the importance of tackling the culture of heavy drinking in Scotland.
“The Scottish Government has made great strides to introduce a comprehensive alcohol strategy, but it will inevitably be less effective without measures to deal with the affordability of alcohol and the proliferation of cheap, high strength alcohol that fuels heavy drinking and causes the greatest harm.
“It is a continuing frustration that legislation to introduce minimum unit pricing of alcohol has been delayed due to the legal challenge by the Scotch Whisky Association and we once again call on them to drop this appeal and allow the introduction of this innovative and world leading public health policy.”
One-in-five older people drink alcohol at unsafe levels
University study looks at the consumption habits of inner-city Londoners
One in five older people who drink alcohol are consuming it at unsafe levels – over 21 units of alcohol for men and 14 units for women each week – according to a study by King’s College London. The research, which was published in BMJ Open, found these unsafe older drinkers are more likely to be of higher socioeconomic status.
The researchers used anonymised electronic GP health records for 27,991 people aged 65 and over in the Borough of Lambeth in London. From these records, they identified 9,248 older people who had reported consuming alcohol, and of these 1,980 people drank at unsafe levels.
They found unsafe drinkers were more likely to be male, younger and have higher socioeconomic status. Men were more likely to be unsafe drinkers than women – 46% of people in the study were male, but they made up 60% of the drinkers and 65% of the unsafe drinkers.
The median alcohol consumption was 6 units per week for all over-65s who reported drinking. However, 5% of alcohol drinkers reported consuming more than 49 units per week for men and more than 23 units per week for women.
Dr Tony Rao, lead author from the Institute of Psychiatry, Psychology & Neuroscience at King’s College London said: “As the Baby Boomer generation become seniors, they represent an ever increasing population of older people drinking at levels that pose a risk to their health. This study shows the need for greater awareness of the potential for alcohol related harm in older people, particularly those of higher socio-economic status, who may suffer the consequences of ill health from alcohol at an earlier age than those in previous generations.”
Alcohol drinkers were also more likely to be ethnically White or Irish, while people from Caribbean, African or Asian ethnicities were less likely to drink. People of White ethnicity formed 59% of the study population, but represented 68% of those who reported drinking alcohol and 80% of unsafe drinkers. 6% of alcohol drinkers (8% of those classified as “unsafe drinkers”) were of Irish ethnicity, despite representing 5% of the study population.
Dr Mark Ashworth, study author from the Division of Health and Social Care Research at King’s College London said: ‘Based on our findings, the elderly who were most at risk were those from the white British population rather than from an ethnic minority, and those who were wealthier and better educated rather than those from a more deprived background.’
The authors caution that results from inner-city London may not apply to other areas of the UK with different demographics. They also note that while the study contains an almost complete sample of older people in the area, people may have under-reported their alcohol consumption to their GP.
‘Alcohol use, socioeconomic deprivation and ethnicity in older people’ by Rao et al is published in BMJ Open.
Podcast
Our monthly podcast features interviews with experts from across the sector.
Bottling Up Trouble: alcohol, workplaces, and the need for change
Tabbin Almond –
Alcohol-freedom coach and author