In this month’s alert
Editorial – September 2018
Welcome to the September 2018 edition of Alcohol Alert, the Institute of Alcohol Studies newsletter, covering the latest updates on UK alcohol policy matters.
This month, the Alcohol Health Alliance launches a postcard campaign to warn about dangers of cheap alcohol. Other articles include: public health chiefs in bust-up with Public Health England over partnership with industry-funded charity Drinkaware; Global Actions report finds corporate social responsibility to be ineffective; and World Health Organization finds 5% of global deaths are down to alcohol.
Please click on the article titles to read them. We hope you enjoy this edition.
COVER STORY – Postcard campaign on cheap drink launched
Calling for duty increases and MUP on alcohol
‘[Megan] tragically passed away on the 1st of January 2014. She’d been to a New Year’s Eve Party the previous night. She’d drank about 1.5 litres of cheap white cider over the space of four to five hours. Tragically she pulmonary aspirated in her sleep in the middle of the night… I support minimum unit pricing to protect our young and vulnerable’
– Joanne Good, talking about her daughter Megan
04 September 2018 – Campaigners, including a bereaved mother, a police officer and a shopkeeper, are backing a national campaign calling for the government to reduce the harm drinking has on society through tackling cheap alcohol.
The Alcohol Health Alliance UK (AHA) is launching a new campaign calling on MPs to end alcohol tax breaks in the upcoming Budget to ease the pressure on the NHS and other public services.
The postcards carry the photos of six people who have been affected by alcohol in different ways: a mother who lost her 16-year-old daughter to cheap white cider; an alcohol harm police officer with Durham Constabulary; a homeless support worker; two frontline doctors; and a Teesside newsagent. You can watch the videos from the Alcohol Health Alliance YouTube page to hear Joanne Good and the others tell their stories.
All feel passionately that more needs to be done to tackle the harms caused by cheap alcohol, but the AHA insists that more help is needed to raise the issue in parliament in order to achieve its main objectives: 1) an increase in alcohol duty by 2% above inflation, and 2) to introduce minimum unit pricing of alcohol (MUP) sold in supermarkets and other off-licence premises.
To raise awareness, the AHA asks that people send a postcard to your local MP urging them to adopt these measures (click here).
FASD a ‘hidden epidemic’
Condition affects more than 15,000 babies a year, says charity
09 September 2018 – At least 2% of people in the UK could be suffering from the long-term effects of their mother drinking alcohol while pregnant.
Not enough is known about foetal alcohol spectrum disorder (FASD), a condition that is often misdiagnosed or missed completely, charities say.
The news comes as charities marked International FASD Awareness Day, calling for more help and advice for vulnerable mothers over what has been termed as a ‘hidden epidemic’ by Adoption UK.
The main symptoms of FASD include growth problems, behavioural issues, learning difficulties and issues with hearing or eyesight. There is no treatment for the condition but its symptoms can be managed.
Because so many cases go undetected it is difficult to know exactly how many people are suffering with the condition.
Sandra Butcher from the charity NOFAS-UK, which is raising awareness of the condition, told Sky News: ‘A conservative estimate would be more than two percent of the population, so here in England that translates into more than 15,000 babies a year.
‘It’s vastly undiagnosed and it’s something that the government is going to have to really get on top of because the problem is that these children are being seen in the NHS through different services but they’re not being properly supported so it’s kind of a waste of resources.’
NOFAS-UK also marked the occasion with the release of an innovative booklet designed to promote wellbeing among children with Foetal Alcohol Spectrum Disorders (FASD), which highlights strategies that can help those living with the condition.
The revelation from NOFAS-UK followed a French study published by Santé Publique which showed that between 2006 and 2013, 3,207 newborns (ie one birth per day on average) presented with at least one health issue related to foetal alcohol syndrome, of which 452 (one birth per week on average) have foetal alcohol syndrome.
It also found that nearly six out of 10 women reported being informed of the risks of alcohol use by the doctor or midwife assigned to them, and that one in 10 reported drank alcohol occasionally during pregnancy.
Pay 3p more for a beer, save lives with an Alcohol Treatment Levy
From the Alcohol Concern website
11 September 2018 – Increasing alcohol duties by 1% would raise around £100 million each year which, invested in alcohol treatment, could save the NHS and other public services around £300 million annually. This would equate to just 5p more for an average bottle of wine and 3p more for a pint of beer – yet would boost alcohol treatment budgets in England alone by 50%.
The charity formed by the merger of Alcohol Concern and Alcohol Research UK says the move will help to address the crisis in alcohol treatment services, saving the public money but, more importantly, saving lives.
Between 2016 and 2018 alone over two-thirds of local authorities cut their alcohol treatment budgets, with 17 local authorities seeing cuts of more the 50%. More than half of the local authorities experiencing the most severe cuts were also in the top two quintiles for numbers of dependent drinkers as a percentage of the total population. This situation is liable to worsen from 2020 when a new funding structure comes into effect.
In 2017, 5,507 deaths in England were directly attributable to alcohol, an increase of 11% since 2006, while hospital admissions caused primarily by alcohol were 17% higher. The total number of hospital admissions for which alcohol was a factor was close to one million, or about 7% of all hospital admissions. Further cuts to treatment budgets will only make things worse.
In addition to the human cost, there is a financial cost. Alcohol costs NHS England alone £3.5 billion each year. A significant proportion of these costs are linked to a relatively small group of individuals with very complex needs, for example mental health problems. Without adequate treatment services this group often fall through the gaps, relying on accident and emergency departments, which costs far more than proper treatment.
Public Health England estimates that for every additional £1 invested in local alcohol treatment provision, £3 is saved.
Dr James Nicholls, director of research and policy development at the charity formed by the merger of Alcohol Concern and Alcohol Research UK, said:
‘While every year the alcohol industry makes around £8 billion from the 4% of the population who drink most heavily, cuts to alcohol treatment services are having a devastating effect across the UK. This is out of balance. We should not leave people with severe alcohol problems unsupported, nor should we leave the 200,000 children living with a dependent parent to fend for themselves. We as a society urgently need to find more money to support essential services. That will help people who drink too much and their families, but it will also save the taxpayer money by avoiding higher costs down the line that could be avoided with treatment.’
Karen Tyrell, Executive Director at Addaction, one of the UK’s leading mental health, drug and alcohol charities, said:
‘We’re thrilled that Steve Brine MP [Parliamentary Under Secretary of State for Public Health and Primary Care] is committed to developing a new alcohol strategy. It’s a real opportunity to set out an ambitious plan to help more people and to counter the damaging effects of hazardous and harmful drinking. But to do that, we need to invest in specialist services for people with an alcohol dependency. At the moment only one in five people who desperately need treatment can get it. That’s not good enough. It heaps pressure on our health services, but most importantly, it means we’re only reaching a fraction of those who need our help.’
MUP boosts alcohol sales for Scottish stores, study says
From Convenience Store
13 September 2018 – Scottish retailers have benefited from an increase in alcohol sales since the introduction of Minimum Unit Pricing (MUP) on 1 May, according to new research from The Retail Data Partnership.
The study of 129 Scottish stores found alcohol sales values increased by 14.9% between May and July this year, when compared to the same period last year, with premium brands gaining share.
The amount that alcohol sales contributed to total store turnover also increased, from 16.31% in 2017 to 18.2% in 2018.
Commenting on the findings, Stephen Burnett, managing director of The Retail Data Partnership, said: ‘It’s probably too early to assess the overall effect of MUP on the number of alcohol units being sold in Scotland. Our figures to date don’t show any real decrease, but we have had an exceptional summer, and soft drinks sales have also been excellent. During Q1 2019 we should be in a better position to evaluate the overall impact of MUP.
‘The warm weather and the World Cup impacted sales across the board in the first half of 2018, with the impact being greater in the rest of the UK,” he continued. ”The rate of increase in Scotland may have been affected by MUP, whilst overall sales as a percentage still remains significantly higher in Scotland.’
The data shows that gin sales leaped hugely in the past year, while Smirnoff vodka gained market share at the expense of Glen’s, indicating a shift towards premium brands as an outcome of MUP.
In a smaller sample of Scottish stores, The Retail Data Partnership also found that most retailers were compliant with minimum unit pricing law, with a few exceptions.
Seven stores were found to be selling Perla Polish 7.6% ABV at less than 50p per unit, while five stores were found to non-compliant when selling Karpackie Super Mocne Polish 9% ABV.
However, Burnett suggested the figures for non-compliant stores could be far greater.
He said: ‘These non-compliance figures may not be representative because our Epos system has a MUP-warning function that alerts retailers when an alcohol price is non-compliant. In stores which don’t have such an alert, compliance may not be as high.’
Jon Ashworth: Alcohol addiction services will no longer be neglected
Health minister’s call comes during National Suicide Awareness Week
14 September 2018 – The Labour Party has promised to strengthen links between addiction services and mental health services if it comes to power, matching one of the recommendations in the Alcohol and mental health report published by the Institute of Alcohol Studies and Centre for Mental Health.
The party plans to create a Substance Misuse Strategy, which would include taking steps to address the links between alcohol misuse, deliberate self-harm and deaths by suicide.
The pledge was made by Shadow Health and Social Care Secretary Jon Ashworth in his address to the National Substance Misuse Conference in Birmingham.
He told the audience: ‘When deaths from drugs are at their highest level, when, as our new research shows, 600,000 are dependent on alcohol needing treatment and over a million hospital admissions a year are alcohol related, when 200,000 are growing up, like I did with a parent who has an alcohol misuse problem, then we have a responsibility to act.
‘Not just for the sake of those individuals whose life has been devastated by drug and alcohol misuse, not just for the children affected but for society as a whole as well.
‘My personal commitment and driving mission, as Health Secretary, would be that drug and alcohol addiction services will no longer be a neglected, under resourced service. The next Labour government will expand substance misuse health services to ensure the most vulnerable in our society are given the support, help, rehabilitation and care they need and deserve.’
87 councils will be cutting alcohol treatment services |
Jon Ashworth also promised at his party’s annual conference that every NHS hospital in England would have an alcohol care team under a Labour Government, a move that would cost £13.5m. It would see all 191 district hospitals have teams of at least three staff to offer specialist help to patients admitted with drink-related problems.
The Labour Party’s commitments to a major programme of expansion of drug and alcohol addiction services comes in the month that figures produced by the House of Commons Library estimate that just 13.3% of the alcohol dependent population in England in 2016/17 underwent treatment – the lowest level since 2011/12 – while the number of those who are alcohol dependent has now topped 600,000.
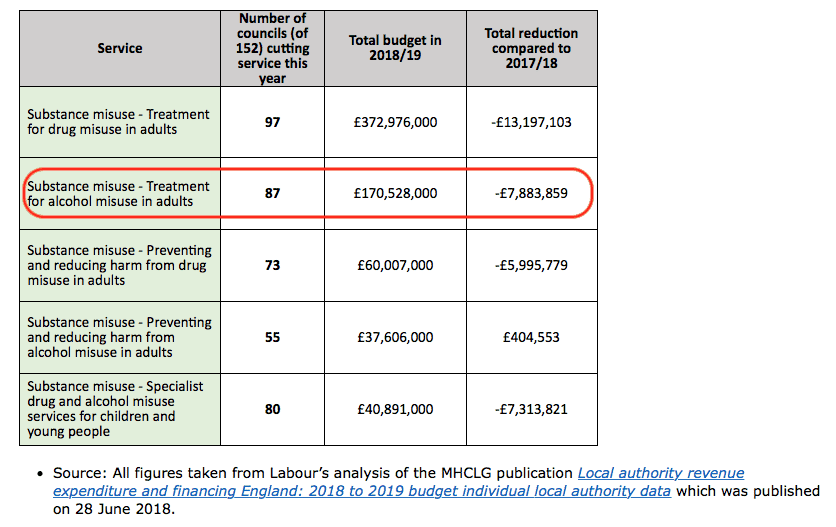
Labour’s analysis of the latest local authority finance figures from 152 councils has also found that substance misuse service provision has fallen, coinciding with the current government’s cuts to addiction budgets. The party’s estimates a further £34m of planned cuts to services this financial year, owing to central government demands for councils to make savings. The majority of councils in the analysis (87) will scrap alcohol treatment services in this period, saving £7.9 million (illustrated).
Responding to the announcement, Andy Bell from Centre for Mental Health said:
‘For too many people with alcohol and mental health difficulties, the help they need is not available when they need it. Mental health and alcohol services too often do not work well together, leaving many vulnerable people with disjointed care or gaps in support.
‘It is vital that the long-term NHS plan brings about a change in this situation nationwide, working in partnership with local authorities to invest in effective integrated support. The costs of ignoring the problem are too great to carry on as we are.’
Alcohol industry CSR actions ineffective
WHO publication Public Health Panorama |
Improving public relations seen as more important than improving public health, say researchers
17 September 2018 – A critical evaluation of alcohol companies corporate social responsibility (CSR) activity has found that fewer than 2% of CSR activities conducted in Europe produced positive health effects.
The findings were published in the Volume 4 Issue 3 of World Health Organization (WHO) Europe’s online magazine Public Health Panorama (illustrated).
Researchers performed a content analysis of 679 CSR actions from more than 3,500 industry-led initiatives and schemes involving producers, trade associations and social-aspects organisations claiming to be in support of the Global strategy to reduce the harmful use of alcohol, adopted by WHO in 2010.
It found that:
- 1.9% of CSR activities were supported by evidence of effectiveness;
- 74.5% did not conform to Global strategy categories; and
- 0.1% were consistent with “best buys” for prevention and control of noncommunicable diseases.
A statistically significant correlation was also found between volume of CSR activities and alcohol industry revenue, as well as market size.
Researchers estimated that the majority of the actions were unlikely to affect more than a small number of people, and that only 2.1% of actions fit the definition of an altruistic approach, in contrast to 82% that were considered to have been designed to further industry commercial interests, such as, for example Heineken introducing the slogan “Enjoy in Moderation” on its labels.
The research team concluded that CSR activities conducted by the alcohol industry in the WHO European Region ‘are unlikely to contribute to WHO targets but may have a public-relations advantage for the alcohol industry’.
NIAAA tweaks alcohol-cancer link understatement
Researcher forces institute to change information on its website
17 September 2018 – An alcohol researcher from the Boston University School of Public Health has successfully forced the National Institute on Alcohol Abuse and Alcoholism (NIAAA) to update information on its website describing the risk of breast cancer associated with moderate drinking.
Dr. Michael Siegel contested the claim that women face an increased risk of breast cancer only if they ‘drink too much’. This is in direct contradiction with the scientific evidence which shows that even light to moderate drinking increases women’s risk of breast cancer.
Dr. Siegel accused the NIAAA of hiding the real risks of alcohol use because it doesn’t want to offend the alcohol companies. Noting that the agency received $67 million from alcohol companies to study the ‘benefits’ of drinking, he asked why it would put millions of women at risk by ‘telling them that there is no increased breast cancer risk unless they drink excessively?’
The NIAAA has since amended its website to say: ‘More than 100 epidemiologic studies… have consistently found an increased risk of breast cancer associated with increasing alcohol intake’, in line with the National Cancer Institute’s messaging.
A spokesman said in a statement to STAT News: ‘We appreciate Dr. Siegel pointing out an area that needed attention and have updated the information on this page accordingly.
‘We are continuing our review of the full website. NIAAA’s goal with the website is to present the most accurate version of the existing data.’
Drink drive limit: Legally safe, but still at risk
TV test proves how dangerous the limit is
19 September 2018 – A televised study testing the efficacy of breathalyser kits has found that the current drink drive limit ‘could be putting lives at risk’.
The experiment, conducted by Professor Antony Moss from London South Bank University and presented by neuroscientist Giles Yeo for BBC2’s Trust Me, I’m A Doctor show (Series 8 Episode 3), found that there were wide variations in several branded breathalysers’ test results.
Six volunteers drinking steadily – consuming between nine and 15 units in one session – and tested at fixed intervals throughout an evening in a pub, remained under the legal drink drive limit (80mg alcohol per 100ml blood) even when they struggled to perform simple tasks, such as walking in a straight line. Yet, all devices overestimated the amount of alcohol in the blood, compared with the police approved kit.
Speaking to presenter Dr Michael Mosley on the show, Richard Allsop, an emeritus professor of transport studies at University College London, and one of the leading proponents behind the UK limit when it was set in 1967, said that studies like this show that the time has come for England and Wales to adopt a lower limit, for the improved safety of road users.
He said that when the limit was originally introduced, the risk of involvement in a collision was roughly double that of a sober driver, but since then, the risk has ‘very much more steeply for the more severe kinds of collision’ than before, to the point that a driver is now 13 times more likely to suffer a fatal crash at the peak of the legal limit threshold than a non-drinking driver.
He also estimated that a 50mg/100ml blood limit would prevent about 25 deaths a year.
The Department for Transport issued the following statement in response to the BBC show’s findings:
‘Drink-driving is completely unacceptable, which is why there are tough penalties and rigorous enforcement in place for those who do this.
‘The government currently has no immediate plans to lower the drink drive limit.
‘However, we keep this policy area under constant review and will always welcome robust and accurate evidence on this subject.’
Diageo bosses challenged on labelling
Alcohol Focus Scotland chief asks tough questions at shareholder AGM
20 September 2018 – The head of a leading alcohol policy charity turned shareholder activist as she confronted executives at the Annual General Meeting (AGM) of drinks company Diageo in London.
Having bought a share in the global drinks giant, Alcohol Focus Scotland Chief Executive Alison Douglas was able to attend the AGM ‘to ask the board why they are failing to provide consumers with the chief medical officers’ (CMO) low risk drinking guidelines on all their products.’
Douglas remarked that the company still carries safe drinking guidelines of up to 21 units a week on its labels, nearly three years since the guidelines were reset to 14 units a week for men and women.
In response, Diageo Chair Javier Ferrán claimed that there was different guidance from different bodies, while admitting that ‘the CMO’s guidelines is the definitive guidance in the UK.’
Douglas told The Times that she repeated the question to Ferrán after the meeting, to which he said that ‘they were a global company and it was very different when different countries have different guidelines’, response she called ‘really disappointing’.
Scotland’s CMO Catherine Calderwood, has called on the alcohol industry to display the updated advice. She said: ‘Providing information on labels is a crucial and effective way to give people health information and advice that informs their choices.’
The Portman Group, which represents UK drinks producers, said that a deadline had been agreed with the UK government for out-of-date information to be removed. A Diageo spokeswoman said: ‘We have signed up to the latest Portman Group guidance on labelling and will implement this by the September 2019 deadline. Our current UK labels promote drinkaware.co.uk, which contains the latest guidelines.’
Alcohol must be recognised as a drug
It should be a priority for all governments, say authors
20 September 2018 – Treating alcohol as a drug will better help inform public health and societal approaches to tackling its ill effects, say two leading public health experts.
Writing in the editorials section of the British Medical Journal, professors Kypros Kypri and Jim McCambridge argue that alcohol must be recognised as a drug in order to ‘strengthen policy responses to harms caused by addiction industries’, and that current attitudes towards alcohol only serves the interests of the alcohol industry.
Kypri and McCambridge also highlight the practices of alcohol companies as having detrimental effects on the public health of citizens. They say that their business model of profiting from addiction is ‘a defining feature of these industries’, along with ‘obstructing the implementation of effective countermeasures’.
In order to reach important long term objectives such as reducing the exposure of children to all psychoactive substances, the authors suggest that alcohol policies must be framed within wider public policies, referring to Sweden’s alcohol, narcotic drugs, doping, and tobacco (ANDT) strategy as a framework that offers the most ‘cohesive’ approach to dealing with negative impacts of substance misuse within a society.
Health agency partnership with Drinkaware sparks row
Fall out with Public Health England over scheme with industry-funded body
21 September 2018 – Public health experts have signalled their opposition to a deal struck between Public Health England (PHE) and a charity funded by the alcohol industry to promote drink free days among middle-aged drinkers.
The executive agency’s announcement of the Drink Free Days initiative led to the resignation of Professor Sir Ian Gilmore from his role as co-chair of the PHE Alcohol Leadership Board.
He wrote of the launch: ‘While people have a right to know about the harms caused by alcohol, we have serious concerns about this campaign itself and the fact that it represents the beginning of a relationship between the alcohol industry and Public Health England.
‘We strongly believe that the alcohol industry should not have a role in providing health information to the general public. The evidence tells us their campaigns are more likely to improve the reputation of global alcohol corporations than improve the health of the nation.
‘The alcohol industry makes two-thirds of its revenue from people who drink at risky levels and the fact that it spends hundreds of millions in promoting its products every year, while it is investing just over £1m in this campaign, shows its true priorities. If it was serious about reducing alcohol harm it would put the low risk guidelines and health warning labels on its products and refrain from opposing measures such as minimum unit price which would be most effective in reducing alcohol harm. In promoting the so-called health benefits of its products and obstructing public policies designed to save lives it is behaving like the tobacco industry.
‘It is our view that PHE is making a serious mistake in partnering with the alcohol industry. Instead, we urge them to work with the wider public health community and others in persuading the Government to take a more evidence-based approach to tackling alcohol harm.’
Several prominent experts also voiced their concerns. Tobacco Control Implementation Board Co-Chair John Britton asked on BBC Radio 4’s Today Programme why PHE wished to risk a repeat of the collaboration made with the tobacco industry in the 1970s and 1980s. This sentiment was echoed in a British Medical Journal (BMJ) article written with Sir Gilmore and Professor Linda Bauld: ‘PHE appear to have fallen victim to the delusion that a new partnership with the alcohol industry will somehow avoid the same fate.’ And another BMJ article penned by Dr Tony Rao warned that the partnership ‘has the potential to capsize public health and all that it represents’.
They were all signatories to a letter, along with more than 50 other royal colleges, charities, and senior medics, that condemned the tie-up as striking a blow to PHE’s credibility, before the deal took place.
However, Chief Executive Duncan Selbie defended the move, saying that although Drinkaware receives funding from alcohol businesses amongst others, ‘they don’t seem to be the alcohol business and they’re fierce of their defence of their independence.’
He continued: ‘Public health must be the place persons are, dwelling the lives that they lead within the locations that they dwell. We want to fulfill them there and be related to them. I make no apology for being clear and direct about this. The marketing campaign might be rigorously and independently evaluated and we will act on its findings no matter they could be.’
This was followed by further criticism of the initiative itself, especially in the messages it gave to those who visited the Drinkaware website. PHE subsequently declared that it was in talks with Drinkaware over the prospect of an audit of its website.
But evidence published in the same week appeared to cast further doubt on the effectiveness of the partnership. The findings of a qualitative systematic review into constructions of alcohol consumption by non-problematised middle-aged drinkers suggested that ‘public health campaigns aimed at reducing alcohol consumption may be more effective if they focus on unacceptable drinking behaviours instead of personal health outcomes.’
Responding to the criticisms, a statement from the health agency read: ‘PHE is steadfast in its ambition to reduce the harms that drinking too much alcohol can cause and we will work together with any partner that speaks to the evidence and shares the same commitment.’
1 in 20 deaths worldwide down to alcohol
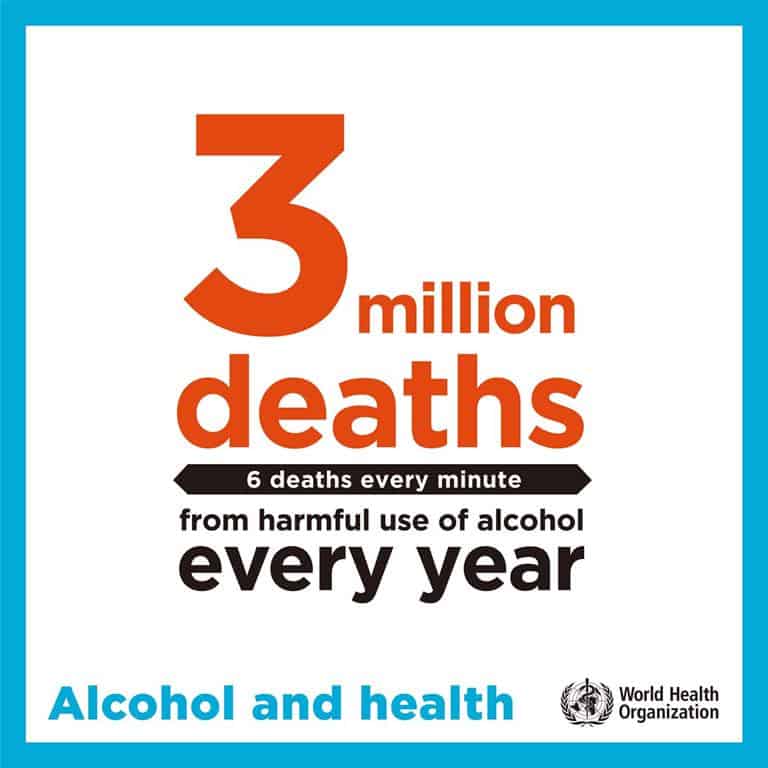 |
New report estimates harmful use of alcohol kills more than 3 million people each year
21 September 2018 – More than 3 million people died as a result of harmful use of alcohol in 2016, 5% of the global disease burden, according a report released by the World Health Organization (WHO).
Global status report on alcohol and health 2018 presents a comprehensive picture of alcohol consumption and the disease burden attributable to alcohol worldwide. It also describes what countries are doing to reduce this burden.
Of all deaths attributable to alcohol, 28% were due to injuries, such as those from traffic crashes, self-harm and interpersonal violence; 21% due to digestive disorders; 19% due to cardiovascular diseases, and the remainder due to infectious diseases, cancers, mental disorders and other health conditions.
Despite some positive global trends in the prevalence of heavy episodic drinking and number of alcohol-related deaths since 2010, the overall burden of disease and injuries caused by the harmful use of alcohol is ‘unacceptably high’ by WHO standards. This is particularly the case in the European Region (14.8% men and 3.5% women) and the Region of Americas (11.5% men and 5.1% women), where the highest prevalence rates exist. Globally, an estimated 237 million men and 46 million women suffer from alcohol-use disorders, which are more common in high-income countries.
Commenting on the findings, WHO Director-General Dr Tedros Adhanom Ghebreyesus said: ‘Far too many people, their families and communities suffer the consequences of the harmful use of alcohol through violence, injuries, mental health problems and diseases like cancer and stroke. It’s time to step up action to prevent this serious threat to the development of healthy societies.’
How much alcohol are people drinking?
The average daily consumption of people who drink alcohol is 33 grams of pure alcohol a day, roughly equivalent to 2 glasses (each of 150 ml) of wine, a large (750 ml) bottle of beer or two shots (each of 40 ml) of spirits.
Worldwide, more than a quarter (27%) of all 15–19-year-olds are current drinkers. Rates of current drinking are highest among 15–19-year-olds in Europe (44%), followed by the Americas (38%) and the Western Pacific (38%). School surveys indicate that, in many countries, alcohol use starts before the age of 15 with very small differences between boys and girls.
Worldwide, 45% of total recorded alcohol is consumed in the form of spirits. Beer is the second alcoholic beverage in terms of pure alcohol consumed (34%) followed by wine (12%). In contrast, more than half (57%, or 3.1 billion people) of the global population aged 15 years and over had abstained from drinking alcohol in the previous 12 months.
More countries need to take action
‘All countries can do much more to reduce the health and social costs of the harmful use of alcohol,’ said Dr Vladimir Poznyak, Coordinator of WHO’s Management of Substance Abuse unit. ‘Proven, cost-effective actions include increasing taxes on alcoholic drinks, bans or restrictions on alcohol advertising, and restricting the physical availability of alcohol.’
Higher-income countries are more likely to have introduced these policies, raising issues of global health equity and underscoring the need for greater support to low- and middle-income countries.
Almost all (95%) countries have alcohol excise taxes, but fewer than half of them use other price strategies such as banning below-cost selling or volume discounts. The majority of countries have some type of restriction on beer advertising, with total bans most common for television and radio but less common for the internet and social media.
‘We would like to see Member States implement creative solutions that will save lives, such as taxing alcohol and restricting advertising. We must do more to cut demand and reach the target set by governments of a 10% relative reduction in consumption of alcohol globally between 2010 and 2025,’ added Dr Tedros.
Reducing the harmful use of alcohol will help achieve a number of health-related targets of the Sustainable Development Goals (SDGs), including those for maternal and child health, infectious diseases, noncommunicable diseases and mental health, injuries and poisonings.
Consumers ‘kept in dark’ over alcohol labelling
AHA report finds fewer than 10% products carry accurate health information
21 September 2018 – The UK Alcohol Health Alliance (AHA) has launched a new report following an audit of 320 alcoholic beverage labels in 12 different locations across the UK in August and September 2018.
Our right to know shows that fewer than 10% of the 320 alcohol products surveyed carry the current low-risk weekly drinking guideline of 14 units a week.
More than two-and-a-half years after the current alcohol guidelines came into effect, most of the 320 products reviewed referred to out-of-date guidelines and carried no health warnings of specific illnesses or diseases. Among the products to carry old information were new drinks, launched after the publication of the current guidelines.
None of the 24 products containing the current guidelines belonged to the global multi-national drinks companies.
The study shows how little progress has been made over the last year since a similar AHA review found only one product contained the correct weekly guideline.
Professor Sir Ian Gilmore, chair of the AHA, said: ‘Once again we see that the alcohol industry cannot be trusted to provide the public with health information. The current system of self-regulation has clearly failed. The industry-funded Portman Group, which advises alcohol producers on labelling, no longer recommends its members include the Chief Medical Officers’ guidelines on labels.
‘We all have the right to know what we are drinking and the fact that alcohol increases our risk of seven types of cancer, liver disease, heart disease and stroke. Few of us know and understand these risks or are aware of the CMOs’ advice. Alcohol companies should be required to display this information along with prominent health warnings, information on ingredients, nutrition and calories on alcohol labels. It’s clear that without government requiring alcohol producers to provide this information, consumers will continue to be kept in the dark.’
Wealthy drinkers more likely to binge
Poorer drinkers still suffer worse health effects
23 September 2018 – People who are well-off are more likely to drink to excess than those in poverty, according to a report published by the Social Metrics Commission.
The findings are part of a report titled A new measure of poverty for the UK, which aims to create a new metric for poverty that accounts for the negative impact on people’s weekly income of inescapable costs such as childcare and the impact that disability has on people’s needs; and includes the positive impacts of being able to access liquid assets such as savings, to alleviate immediate poverty.
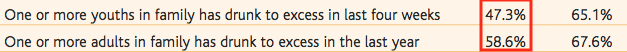
By this new standard, 67% of those on better-off incomes know of one or more adults in family who have drunk to excess in the past year compared with 58% of those classified as living in poverty (illustrated below). Yet, as health experts often say, it is the poorest in society who are ‘at greater risk of alcohol’s harmful impacts on health’, despite drinking less than their wealthy counterparts. Drug addiction / problem alcohol use was identified as one of the nine major factors of the lived experience in those in poverty.
 |
Podcast
Our monthly podcast features interviews with experts from across the sector.
Gambling industry harms and parallels with the alcohol world
Will Prochaska –
Coalition to End Gambling Ads

