In this month’s alert
Editorial – July 2017
Welcome to the July 2017 edition of Alcohol Alert, the Institute of Alcohol Studies newsletter, covering the latest updates on UK alcohol policy matters.
This month’s issue sees the Scottish Government go to the UK Supreme Court in the latest episode of a long-running battle against the Scotch Whisky Association over the legality of its minimum unit pricing legislation. Other articles include: the Foundation for Liver Research makes the ‘financial case’ for action on liver disease; a new National Drug Strategy sparks a debate about alcohol; government department cosies up to the wine and spirits lobby at a roundtable meeting; and an Alcohol Health Alliance survey find that pocket money prices for alcohol continue one year on.
Please click on the article titles to read them. We hope you enjoy this edition.
TOP STORY: Supreme Court MUP showdown: Scots Govt versus Big Whisky
Industry lawyers make last-ditch attempt to scotch legislation
Five years after Scotland legislated for Minimum Unit Pricing (MUP), lawyers met at the UK Supreme Court in London to discuss whether their legislation is incompatible with European Union law and therefore unlawful under the Scotland Act 1998.
The two-day hearing may turn out to be the final chapter in a long-running court case between the Scottish Government and an opposition led by the Scotch Whisky Association (SWA).
Given the right to appeal the 2016 ruling of the Scottish Court of Session, the SWA’s lawyers brought the case to be considered by seven justices at the UK’s highest court.
Led by Lord Neuberger, judges pored over the details of the 2013 ruling of the Lord Ordinary, which rejected the SWA appeal in the first instance at the Scottish Court of Session in Edinburgh. The case has since been taken to the European Court of Justice – which ruled that it was for the domestic courts to decide – and then back to the Scottish Court of Session, whose judges again declared MUP to be lawful.
A law of “national public importance”
Some legal experts in Scotland who have been following the case have stressed the potential implications of the verdict to be delivered from the current appeal. Emma Boffey, a solicitor at law firm CMS, told The Financial Times that the appeal is one of the “most significant” public law cases to be heard before the UK Supreme Court this year.
“It is of national public importance: the decision in the case will have an immediate and lasting impact on the direction of public health policy in Scotland.
“The Scottish Government’s position has been that the societal problems caused by excessive alcohol consumption in Scotland are so significant that groundbreaking measures are required,” said Boffey.
Public health NGOs are also taking a very keen interest in the case for this reason. In an article for The Herald, Alcohol Focus Scotland chief executive Alison Douglas said: “Preventing alcohol harm requires regulation not simply education. Alcohol producers and retailers need to accept that the products they make and sell are toxic, addictive and carcinogenic so it’s absolutely right that controls are in place to minimise the harm caused.
“We don’t want Scotland to be known for heavy drinking. That’s not something to be proud of. We should be known for our progressive approach to improving health, creating better communities, and reducing inequalities. Minimum unit pricing is the biggest public health breakthrough since the ban on smoking in public places. It will save many lives and improve many more.”
A “quiverful” of options
Acting for the SWA, Aidan O’Neill QC claimed that MUP plans were “too much of a blunt instrument to be justifiable as a matter of health and protection of life of humans”, and that there were a “quiverful” of other taxation measures or excise reforms that would be fairer and legal under EU law, and also mean that the extra taxes could be spent directly on health and anti-poverty measures.
However, defending the legislation, James Wolffe QC, Scotland’s Lord Advocate, argued that the ECJ’s ruling considered that as an issue, but was satisfied that the aforementioned interference was justified on the grounds that it pursued the objective of protecting health and life by reducing, in a targeted way, both the consumption of alcohol by consumers whose consumption was hazardous or harmful, and also, more generally, the population’s consumption of alcohol.
“It effectively targets those who will benefit most, namely hazardous and harmful drinkers. There is a strong evidence base that it will be an effective intervention.”
Implications
Scottish Health Action on Alcohol Problems (SHAAP) hope that the judges’ decision will finally signal the go-ahead for the Scottish government to implement MUP. The NGO estimates that in the 5 years that the law has been delayed, approximately 5,700 heavy drinkers reliant mainly on cheap vodka and white cider have died as a result of alcohol-related causes, and that MUP – a popular policy among the Scottish public – would be one of the most effective measures in helping problem drinkers to cut down on their risky consumption.
SHAAP director Dr Eric Carlin said: “As representatives of front line medical practitioners and public health, we have praised the Scottish Government’s continued commitment to MUP as a key policy that, along with other evidence-based policies, will reduce alcohol harms in Scotland. We have consistently been shocked by the disregard for Scottish lives by the global alcohol producers, fronted by the Scotch Whisky Association, who have used financial muscle and spurious, changing arguments to block the implementation of MUP.
“The policy became law in 2012, without any opposition in the Scottish Parliament. We keenly await the Supreme Court judgement, which we hope will come soon. We are confident that their Lordships will favour this life-saving policy, which we hope will now be implemented in Scotland, with as little delay as possible.”
As James Morris writes in Alcohol Policy UK, the MUP legal ruling also has significant implications for the Welsh and Irish governments, that wish to implement similar measures in their jurisdictions. In England, government ministers have been sketchy on the issue following the infamous 2012 U-turn, but have largely insisted they have not ruled out the policy.
Although the date of the Supreme Court’s ruling is not yet known, many involved in the field will be hoping that the verdict proves final.
You can follow the Soundcloud link to hear SHAAP chair Dr Peter Rice offer a brief history of Minimum Unit Pricing in our latest Alcohol Alert podcast.
Hepatologists make ‘financial case’ for action on liver disease
Doctors claim heavy drinking will kill 63,000 people over next five years
The Foundation for Liver Research, an organisation of leading hepatologists, has brought together a range of statistics on the economic, social and fiscal impact of liver disease in its new report: ‘Financial case for action on liver disease’. Endorsed by the Lancet Commission on Liver Disease, the report argues that these numbers demonstrate an urgent need for concerted preventative action to tackle alcohol misuse, obesity and viral hepatitis. Proposed policy solutions include:
- A minimum unit price for alcohol
- The reintroduction of the alcohol duty escalator to ensure alcohol taxes rise by 2% above inflation each year
- A specific tax on high strength ciders between 5.5% and 7.5% ABV to target ‘white ciders’
- Trading hours for off-trade retailers to be restricted to 10am-10pm, and limits to on-trade sales after midnight
- Strengthened regulation of alcohol marketing and advertising, including banning sports sponsorship, restricting cinema adverts to 18 certificate films, and a watershed for TV advertising
The Foundation for Liver Research builds its case on the basis of figures from a range of sources, which show among other things that:
- The societal cost of alcohol in England and Wales has been estimated between £21 billion (UK Government Cabinet Office) and £52 billion (Public Health England)
- Without further action, between 2017 and 2022, alcohol-related illness in England is projected to cause 63,000 deaths and cost the NHS £17 billion (University of Sheffield / Cancer Research UK)
- 167,000 years of working life were lost in England in 2015 (Public Health England)
- 57,940 claimants of government sickness/disability benefits had alcohol misuse as their primary medical condition (Department of Work & Pensions)
- Alcohol-related crime has a social cost of £13 billion a year in England and Wales (Home Office)
Professor Roger Williams, Director of the Foundation for Liver Research, and Chairman of the Lancet Commission on Liver Disease argued:
“Liver disease is a public health crisis that has been steadily unfolding before our eyes for a number of years now and the Government will have to take robust public health action if its main causes (alcohol misuse, obesity and viral hepatitis) are to be controlled. Our new report strengthens the argument for intervention by revealing the full and alarming extent of the financial costs associated with inaction in these areas and setting out the economic benefits of addressing these risk factors.
“Three years ago, the Lancet Commission on Liver Disease created a blueprint for improvement, supported by the clinical community, setting out a range of targeted measures to reduce the burden of ill health in these areas. Yet we are still missing prioritisation, funding and drive to implement the Commission’s recommendations. We urge the Government to take immediate steps to halt and reverse the crisis in liver disease.”
Commenting on the findings in The Guardian, Katherine Brown, director of the Institute of Alcohol Studies, accused the government of not doing enough to limit alcohol-related harm, given that reducing avoidable deaths from a range of life-threatening conditions is a key target of government health policy. (read full quote below).
Raised cancer risk for majority of moderate European drinkers
Two drinks a day increases risk – UK above average level
Citizens across the European Union (EU) are consuming an average of two alcoholic drinks per day, placing drinkers at a 21% increased risk of developing colorectal cancer, in addition to other digestive cancers, a report finds.
Launched by United European Gastroenterology (UEG), the report ‘Alcohol and Digestive Cancers Across Europe: Time for Change’ revealed that the average daily intake of alcoholic drinks was ‘moderate’ (between 1 and 4 drinks per day) in all 28 EU states, placing its citizens at a heightened risk of both colorectal and oesophageal cancer. Anyone having four or more drinks a day is at risk of three other cancers: liver, gastric and pancreatic cancer.
Lithuania topped the list with an average per person consumption of 3.2 drinks per day. Britons consume an above-average 2.1 alcohol drinks every day (equal to 26.7 grammes daily or 12.3 litres of pure alcohol annually), ranking the country 8th highest of all Member States.
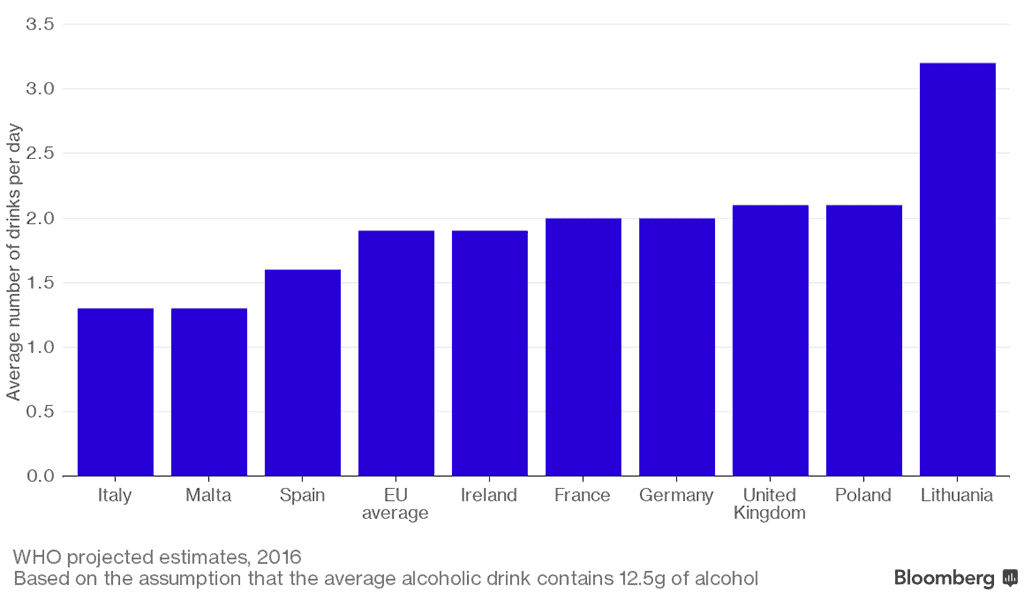
Given such figures, the Alcohol Health Alliance (AHA) has urged ministers to push for alcohol manufacturers to be mandated to put health warnings on the labels of cans and bottles, to organise sustained campaigns alerting the public to the dangers of drinking and to introduce minimum unit pricing, in order to reduce overall consumption and alcohol-related health harms.
“These findings show clearly that because of current consumption levels in Britain we are some of the most at-risk people for developing these types of cancers,” said AHA chair Sir Ian Gilmore.
“This is not surprising when enough alcohol is sold in England and Wales for every drinker to consume 50% more than the weekly limit recommended by the UK’s chief medical officers.
“Alcohol is a group one carcinogen and while the evidence shows any level of drinking increases cancer risk, this risk increases in line with the level of consumption,” he added.
The report itself identified accessibility as having a “direct effect on misuse”, blaming the 24-hour availability of alcohol in the UK for “providing greater opportunity for alcohol misuse, particularly for high-risk drinkers, with serious health risks as a result”, ultimately suggesting sales restrictions on alcohol in the evenings to curb the problem.
The European alcohol endemic – a “deeply embedded” problem
The UEG press release states that: “Alcohol consumption across the European region is higher than in any other region in the world, with over one-fifth of the European population over the age of 15 drinking heavily at least once a week. As a result, the continent suffers from the highest proportion of ill health and premature death directly linked to alcohol.
“Despite high levels of consumption throughout Europe, research shows that as many as 90% of people are unaware on the link between alcohol and cancer.”
Professor Markus Peck, a member of UEG’s public affairs committee and the ex-secretary general of the European Association of the Study of the Liver, said: “One of the main challenges in addressing high drinking levels is how deeply embedded alcohol consumption is within the European society, both socially and culturally.
“Political action like minimum unit pricing and reducing access to alcohol needs to be taken now to prevent many future casualties.”
Professor Helena Cortez-Pinto of the European Association for the Study of the Liver (EASL), agreed, remarking that minimum pricing had been “proven to be extremely effective in Canada” and that, subject to the result of a long-running legal case, Scotland will be next and “hopefully the rest of Europe will follow shortly.”
Estonia to make drinking an EU health priority
The UEG wants reduction of alcohol harm to be a key priority of the Council of the European Union under the new Estonian presidency. This was reflected in the statement that the Estonian Minister of Health and Labor (Jevgeni Ossinovski) gave in Brussels, as reported in the Baltic Times.
Introducing the priorities of the Estonian EU presidency to the European Parliament’s Committee on Environment, Public Health and Food Safety, Ossinovski said: “As the presidency, we consider it important to open discussion on the labelling of alcoholic beverages, as it is obviously a cross-border aspect, where more can be achieved at the level of the European Union.”
The minister also stressed how alcoholic beverage products lack the safety requirements that have been put in place for other consumer products, from toys, and cosmetics, to tobacco and pharmaceuticals. “According to the estimations, the yearly societal costs of alcohol consumption in the EU can reach up to €372bn”, he added.
Estonia will be organising a conference on how to tackle the cross-border aspects of the harmful use of alcohol on October 30 and 31.
DEFRA invites industry to roundtable
Event “first in a series” of briefings to government department
The Wine & Spirits Trade Association (WSTA) has been called upon to brief ministers from the Department for Environment, Food and Rural Affairs (DEFRA) on “what the drinks industry needs to maintain its number one global position and continue to grow”, according to Drinks Retailing News.
WSTA chief executive Miles Beale attended a roundtable event led by Secretary of State Michael Gove, the first in a series of meetings to bring together the people and influencers at the cutting edge of the UK’s food and drink sector.
Beale said: “The food and drink roundtable has given us the opportunity to get together with government and make them understand our concerns and highlight better ways of working together.
“As a follow up to the meeting I have also written a letter to Mr Gove spelling out what Government needs to do to protect The UK’s status as the number one global hub for wine imports and the world’s biggest exporter of spirits.
“The UK drinks industry is incredibly important to the economy and we need to ensure government is listening to the industry to ensure we maintain free flows of trade.”
Web retailers serve up poor ID test results
Majority of online vendors do not verify proof-of-age on delivery
Retailers sold alcohol to nearly one in six teenage mystery shoppers in 2016 without asking for proof of age, according to new data from Serve Legal.
The retail age check auditor said its testers – 18 and 19-year-olds posing as under-age customers – undertook nearly 43,000 alcohol sales tests in supermarkets, convenience stores and petrol stations across the UK in 2016.
Age ID was requested in 83% of visits before alcohol was handed over. Supermarkets were the highest-performing retailers, passing 84% of all tests in 2016, 3 percentage points down on 2015. The pass rate also fell slightly for convenience stores over the same period, from 83% to 82.5% of alcohol ID check tests in 2016.
Geographically, Scotland maintained its historical position of achieving the highest overall alcohol test pass rate in the UK with retailers passing 87% of age check tests in 2016. Northern Ireland was the poorest performer with a pass rate of 72%.
Online shopping poses a particular risk for under-age sales. In more than 500 age check tests among online retailers undertaken by Serve Legal in 2016, only 41% of young mystery shoppers were asked for proof of age at the point of delivery.
Serve Legal director Ed Heaver said: “We are seeing far too few online retailers committing to age check testing at the point of delivery.
“Even the most stringent age check measures at the point of online purchase do not prevent a delivery driver failing to ask for proof of age before handing over age-restricted goods on the doorstep or leaving goods in a porch or shed for an under-age buyer to collect.
“Responsible retailing – and the law supporting it – should apply to every link in the chain. The nature of the tight delivery schedules driven by the so-called gig economy is almost certainly a factor in the low levels of age checks revealed by our data.”
Serve Legal conducts around 100,000 tests a year on retailers of age-restricted products across the UK, where its (young-looking 18 and 19-year-old) testers record key information about their visit, including whether ID was requested, a description of the server and a till receipt. Accepted forms of ID are: passports, photocard driving licences, and PASS-accredited IDs.
“Rigorous, regular testing for age-restricted sales see compliance levels improve, which reduces the risk of alcohol products getting into the hands of children. It should be an integral parts of retail training and operational best practice, not a panic purchase after a sting by trading standards or the police,” Heaver added.
MP pledges to equalise drink-driving law after boy’s farm death
Rules different for private roads compared with public ones
A government minister has pledged to revisit the law on drink-driving on private land, a grey area of the law where a recent fatal accident case could only be prosecuted by the Health & Safety Executive (HSE) under the Health and Safety at Work Act.
The pledge came after Alec Shelbrooke, MP for Elmet and Rothwell, raised the issue in the House of Commons on 13 July. His intervention followed the case of 11-year-old Harry Whitlam, who was killed in August 2013 by a tractor driven by a drunk employee on a farm near Leeds.
In response, transport minister John Hayes said that the penalty for an illegal action should not depend on where it happens, and that: “I will consider how we might address this, including the possibility of future legislative reform.”
He added: “It is important that we get the reform right, and that we do not rush and make errors in how we frame that kind of legislation.”
The commitment follows the HSE’s prosecution of Gary Green over Harry’s death, for breaching Section 3(2) of the Health and Safety at Work Act in December last year. Green was sentenced to 16 months and 2 weeks in prison. As the law stands, he could not be prosecuted for death by dangerous driving while under the influence of drugs or drink, as he was not driving on a public road.
The Crown Prosecution Service apparently reviewed the case, but decided that Green’s actions did not pass the threshold for a charge of manslaughter by gross negligence. However, if charges could have been brought under section 3 of the Road Traffic Act 1988, then the maximum penalty would have been 14 years’ imprisonment.
According to Shelbrooke, the CPS had informed him that Green’s sentence under such a charge would have been in the region of 6 years. Shelbrooke also highlighted that the family had to wait some 17 months before the HSE was able to prosecute the case.
Last December, Leeds Crown Court heard that the self-employed farm worker was found to be 2.5 times over the legal drinking limit after the fatal accident in August 2013. Harry had been a regular visitor to Swithens Farm, especially during the school holidays, as his mother worked at the café. He would be accompanied if he was in a section that was closed to the public.
An HSE investigation found that the tractor was reversing when it struck Harry, who was walking towards another worker at the time.
Speaking after the hearing, HSE Inspector Julian Franklin said: “This is an extremely tragic case. Harry was a young boy whose life was cut short by the reckless behaviour of Gary Green. Drink driving legislation does not apply on private land but it does not mean you can blatantly disregard the health and safety of those around you when driving heavy and dangerous machinery.”
Quoted by Shelbrooke in his House of Commons speech, Harry’s mother Pam Whitlam said that she hoped “Whitlam’s Law” could be a way of making sure her son’s death made a difference.
Originally published in Health and Safety at Work.
Mixed national outlook from local alcohol consumption data
Survey “reinforces the need to provide intelligence at the local authority level”
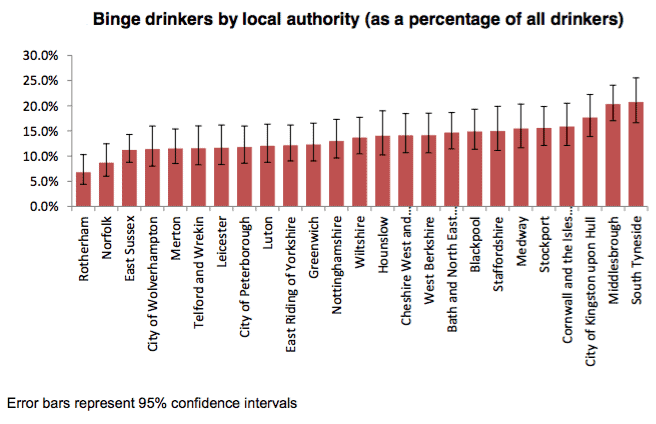
Data commissioned by Public Health England have revealed a “wide variation in behaviour between different local authorities.”
Pollsters IPSOS MORI collected information from a sample of 25 local authorities chosen to provide coverage of all regions and types of local authority, in response to a noted lack of reliable information about alcohol consumption at the local level, “primarily because of the prohibitive cost of collecting data for all local authorities.”
There were a total of 9,683 responses to survey questions over a 2-month period (29 February to 25 April 2016) using a postal survey methodology, plus results from 604 face-to-face interviews in Middlesbrough and East Sussex.
Results
PHE’s authors wrote that the results revealed a “wide variation in behaviour between different local authorities” and that “even local authorities which were geographically close such as Leicester and Nottinghamshire had different profiles of drinking behaviour.” Their findings provide “further evidence of the need to measure alcohol consumption at a local level and the limitations of averaged regional data to inform local planning.”
One example of the range between local authorities involved rates of abstinence. Abstention rates varied from 14% in Stockport to 38% in Leicester (illustrated below). Women were more likely to abstain than men (24% compared with 19%).
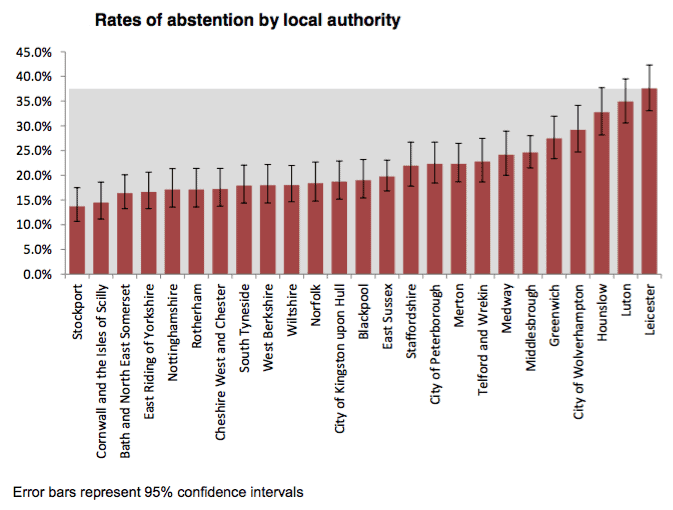 |
source: Public Health England
At the other end of the scale, binge drinkers (defined as women drinking more than six units and men more than eight units in a single drinking occasion on a regular and frequent basis) ranged from 7% in Rotherham to 21% in South Tyneside (illustrated below).
|
Alcohol Use Disorders Identification Test (AUDIT) scores seemed to correlate with hazardous drinking behaviours; adults in the highest AUDIT group (who show signs of possible alcohol dependence) drank on average 59 units of alcohol a week, were more likely to consume strong beer or cider, and to drink most of their alcohol at home.
However, AUDIT scores also reduced with increasing age, a positive trend over the lifecycle.
10.4% of respondents had participated in a campaign to reduce alcohol consumption with 70% of those specifically citing Dry January as their campaign of choice. The likelihood of participating in such campaigns increased by AUDIT group – a third of respondents in the highest risk AUDIT category had participated in a campaign to reduce their drinking.
Those with parental responsibility for children in their household were less likely to be drinking at increasing and higher risk than those without (84% compared with 79%).
Awareness of Chief Medical Officer’s guidelines on low risk drinking rises with age – overall, roughly 30% of respondents were aware of the guidelines but didn’t know the details.
Limitations
The local consumption survey was designed as a pilot covering a sample of local authorities which were chosen to provide coverage of all regions and type of local authority. The survey aimed to provide reliable consumption estimates for a large, representative sample of local authorities; to provide a mechanism for validating local authority estimates of dependent drinkers produced and other modelled estimates of alcohol consumption by local authority, and; to assess the feasibility of using data from sampled local authorities to infer consumption patterns in local authorities which were not sampled.
PHE acknowledged two important limitations with the data. Firstly, the sample size was 20% overall, low compared to the Health Survey for England, which achieves a response rate around 60%. It was also skewed in favour of households with older people compared those with young people. Secondly, UK household surveys underestimate population-level alcohol consumption to the tune of between 55% and 60% of the total consumption implied by actual sales data. It is therefore reasonable to assume that the data collected for this survey will underestimate true alcohol consumption levels.
There is also a further difficulty in being able to run surveys like this for all upper tier local authorities over time; the costs of doing so are estimated to be approximately half a million pounds, therefore it seems unlikely that any one body would be able to fund this in the foreseeable future.
Commenting on the report’s findings, PHE said: “In order to take effective action on alcohol-related harms and to ensure this action is appropriate, we need to understand levels and patterns of alcohol consumption which can vary significantly between different sub-populations.
“The results from the survey have provided clear evidence of variability between local authorities and the need to have intelligence at that level.”
New National Drug Strategy released – but what about alcohol?
2017 action plan sparks debate over “most harmful drug”
Politicians and NGOs have made fresh calls for a new alcohol strategy in the wake of the government’s release of a National Drug Strategy for England and Wales.

|
Home Office minister Sarah Newton MP (Truro and Falmouth) (Con) was forced to defend the government’s position in a parliamentary debate over the issue, insisting that she would “not be drawn into a wider debate about the current legal framework around alcohol, because we are here today to talk about our drugs policy.”
This did not stop Newton being questioned about the inclusion of alcohol in the strategy in the context of dependence, but not in terms of its damage. When Norman Lamb MP (North Norfolk) (Lib Dem) said that “evidence clearly shows that the most dangerous drug in terms of harm is alcohol”, Newton replied:
“I would not agree that alcohol is the most dangerous drug, as we can see if we look at the substances we are restricting… I fully accept, as the Government do in the modern crime prevention strategy, that the misuse of alcohol has dramatically harmful effects and contributes to crime, but alcohol taken in moderation is not a harmful drug.”
The latter point was immediately challenged by Thangam Debbonaire MP (Bristol West) (Lab), who said: “[Newton] said… that there is such a thing as a safe level of consumption of alcohol, but that is not what the National Institute for Health and Care Excellence [NICE] guidelines say. The NICE guidelines are clear and accurate: there is no safe level of consumption of alcohol… Evidence is available that shows just how much more harmful alcohol is than any other drug.”
Debbonnaire went on to reiterate Lamb’s comments, saying that the strategy “virtually, although not completely, ignores the most harmful drug. I say respectfully to the Minister that alcohol is a drug, and one that is entirely legal.”
As James Morris notes in Alcohol Policy UK, the new drugs strategy does in fact refer to drugs and alcohol throughout. However, in the context of treatment for alcohol problems it may be seen as reflecting national alcohol ambitions for treating and preventing all subtance dependence.
Fiona Bruce MP (Congleton) (Con), who is chair of the All Party Parliamentary Group (APPG) on Alcohol Harm, pointed out that in the context of mortality rates, a new alcohol strategy might be the best solution.
Bruce said: “I recognise that the strategy contains recommendations for joined-up action on alcohol and drugs, and that areas of the strategy apply to both. As we have heard this afternoon, however, we need to do more. Statistics illustrate the extent of the harm caused by alcohol. In 2015 there were 2,479 deaths from drug misuse. In the same year, there were 23,000 alcohol-related deaths. Drug deaths equate to only 10% of the number of deaths caused by alcohol… It is vital that we recognise the need to review the alcohol strategy.”
Diane Abbott MP (Hackney North and Stoke Newington) (Lab) agreed, quoting Alcohol Health Alliance UK chair Professor Sir Ian Gilmore in calling for “a dedicated strategy on alcohol which recognises the breadth of harm done by alcohol.”
The 2017 Drug Strategy contains a section on alcohol, which states: “While the focus of this Strategy is on drugs, we recognise the importance of joined-up action on alcohol and drugs, and many areas of the Strategy apply to both, particularly our resilience-based approach to preventing misuse and facilitating recovery. Alcohol treatment services should be commissioned to meet the ambitions set out in the Building Recovery chapter that are relevant to them, and in line with the relevant NICE Alcohol Clinical Guidelines. Commissioning of alcohol and drug treatment services should take place in an integrated way, while ensuring an appropriate focus on alcohol or drug specific interventions, locations, referral pathways and need.
“In addition, local authority public health teams should take an integrated approach to reducing a range of alcohol related harm, through a combination of universal population level interventions and interventions targeting at risk groups. The Modern Crime Prevention Strategy 2016 highlights alcohol – as with drugs – as a key driver of crime and sets out a range of actions to tackle alcohol-driven crime.”
James Morris observes that despite the rhetoric, the strategy is not a ‘drug and alcohol strategy’, and “some argue that there are many issues with providing alcohol treatment – or indeed strategies – under the same roof.”
Such concerns were voiced by the Cross-Party Parliamentary Group on Drugs, Alcohol and Justice, which convened the week before (12 July) to discuss the UK drug treatment landscape, in the face of the UK’s position as the drugs overdose capital of Europe. Responding to the findings of an investigation into the funding cuts to councils across the UK, the Group put forward an evidence based ‘Charter for Change 2017’, an action plan intended to guide future steps in the field.
The Charter identifies 10 action points relating to drug and alcohol policy, including calls for the Government to publish both a Drug and an Alcohol Strategy. The Charter also puts forward the proposal for a dedicated Government Minister for drug and alcohol policy.
The Group heard from speaker Kevin Jaffray of the Naxolone Action Group who spoke of the strain the £85m cuts to public health budgets have placed on treatment services. In discussion of the report ahead of the event, Jaffray discussed the impact these cuts have made in The Guardian, noting the sharp drop in access: “Only one or two people in each area was [sic] getting awarded the funding to go into rehab and a hell of a lot more people than that were requesting it.”
In line with this, the Charter discusses treatment services for drugs and alcohol, including the need to “ensure everyone in recovery from drug and alcohol problems has opportunities to rebuild their lives…” A key discussion centres around the funding cuts suffered by Local Authorities (LAs), which has seen many reduce treatment services available to those in recovery. As such, the Charter proposed a mandate for provision of such services by LAs, and to ensure these authorities “provide adequate resources” from these services.
The Group is scheduled to next meet in the autumn.
Pocket money prices for alcohol continue one year on
Survey is yet more evidence of the need for minimum unit pricing
A survey published just days before the UK Supreme Court hears a case to decide whether introducing a minimum unit price for alcohol is legal shows that cheap, strong alcohol continues to be sold for pocket money prices up and down the country.
One year ago, a survey of alcohol prices across the UK found an abundance of cheap drinks being sold in shops and supermarkets, with high-strength cider available at the lowest prices.
A follow up review carried out this month in England, Scotland and Wales has found that these cheap prices remain largely unchanged, with products across the market still falling well below the 50p per unit mark recommended by health and alcohol bodies.
Both price reviews were carried out by the Alcohol Health Alliance UK (AHA), a group of medical royal colleges, alcohol organisations and health bodies. In this year’s review, the AHA found that cider continued to be sold at the lowest prices overall, with 3-litre bottles of 7.5% ABV cider (containing the equivalent of 22 shots of vodka) moving from £3.49 in 2016 to just £3.59 in 2017 (or 16p per unit). At that price, for the cost of a small latte in Starbucks it is possible to buy more alcohol than the weekly recommended limit of alcohol.
The cheapest wine surveyed in 2016 was found to be even cheaper in 2017, and available for just 31p per unit.
Cheap, high-strength alcohol is known to be predominantly drunk by the most vulnerable groups, including children and the homeless, and a minimum unit price for alcohol of 50p per unit was passed by the Scottish Parliament in 2012, only to be held up by a legal challenge from sections of the alcohol industry. The Welsh government recently announced it will legislate for minimum unit pricing, and the Northern Ireland Executive has also expressed its desire to implement the policy.
The AHA said that the figures provide yet more evidence for the need for minimum unit pricing to be introduced across the UK. Professor Sir Ian Gilmore, chair of the Alcohol Health Alliance UK (AHA), said:
“It is frankly unacceptable that it is possible to buy enough alcohol to exceed the new recommended alcohol guidelines for the price of a high street coffee. We need minimum unit pricing for alcohol so that the damage being done by the cheapest products to the most vulnerable in society can be brought to an end. We hope and expect that following the hearing on minimum unit pricing next week, Scotland will be given the green light to introduce the policy.
“With the recent announcement that the Welsh government also intends to legislate for minimum pricing, and a previous commitment to MUP from the Northern Ireland Executive, it is imperative that the UK government now legislates for MUP, so that England does not get left behind the rest of the UK. The Westminster government expressed its intention to introduce minimum pricing five years ago, but has still not delivered on this commitment.
“The evidence is clear – minimum unit pricing would save lives, reduce hospital admissions and cut crime. In addition, it would disproportionately benefit the poorest groups. Studies show that 8 out of 10 lives saved through minimum pricing would come from the lowest income groups.
“With alcohol-related hospital admissions at record highs, and liver disease rates on the rise, we can’t afford for alcohol to remain at such low prices.”
|
|
Premises |
Location |
Brand |
Strength (% abv) |
Price |
Price per unit |
|
Beer |
|
|
|
|
|
|
|
2016 |
Aldi |
North East of England |
Own brand (4x440ml) |
2% |
£0.89 |
25p |
|
2017 |
Tesco |
Cardiff |
Everyday Bitter (4x440ml) |
2.1% |
£1.00 |
28p |
|
|
|
|
|
|
|
|
|
Cider |
|
|
|
|
|
|
|
2016 |
Bargain Booze |
London |
Frosty Jack’s (3L) |
7.5% |
£3.49 |
16p |
|
2017 |
Iceland |
London |
Frosty Jack’s (3L) |
7.5% |
£3.59 |
16p |
|
|
|
|
|
|
|
|
|
Vodka |
|
|
|
|
|
|
|
2016 |
Independent |
North East of England |
Krakus (70cl) |
40% |
£10.00 |
36p |
|
2017 |
Lidl |
Scotland/London |
Rachmaninoff (70cl) |
37.5% |
£9.97 |
38p |
|
|
|
|
|
|
|
|
|
Wine |
|
|
|
|
|
|
|
2016 |
Aldi |
North West of England |
Own brand (75cl) |
13.5% |
£3.29 |
32p |
|
2017 |
Aldi |
Scotland |
Own brand (75cl) |
13.5% |
£3.09 |
31p |
|
|
|
|
|
|
|
|
|
Perry |
|
|
|
|
|
|
|
2016 |
Asda |
North East of England |
Still Lambrini (3L) |
7.5% |
£4.25 |
19p |
|
2017 |
Lidl |
Wales |
Baywood (3L) |
7.5% |
£4.29 |
19p |
|
|
Aldi |
Wales |
Grove Manor (3L) |
7.5% |
£4.29 |
19p |
Comparison of cheapest products found – 2016 and 2017
Fieldwork for the 2017 price review was carried out in Cardiff, London, Scotland and the North East of England in July 2017. Full details of the 2016 price review can be found in the AHA’s report, ‘Cheap alcohol: the price we pay’.
Originally posted on the Alcohol Health Alliance website.
Majority of forces at increasing risk of alcohol-related harm
First time AUDIT-C has been used on large scale in military population
A one-off report from the Ministry of Defence has shown that three-fifths of armed forces are “potentially at increasing risk or above” of alcohol-related harm.
Alcohol Usage in the UK Armed Forces reports on the Ministry’s initiative to introduce an alcohol screening tool (the Alcohol Use Disorders Identification Test-Consumption (AUDIT-C)) and brief advice (an Alcohol Brief Intervention) for all UK Armed Force Personnel attending routine dental inspections in the year to 31 May 2017.
Of the 109,459 staff who completed the questionnaire, 61% (66,958) of armed forces personnel scored 5+, indicating that they may potentially be at increasing risk or above of alcohol-related harm.
2% (2,502) of personnel scored 10–12, indicating that they may potentially be at increasing or higher risk and should be advised to see their GP. This included 217 personnel who scored 10–12 that had a referral to their GP recorded in their medical record (illustrated below).
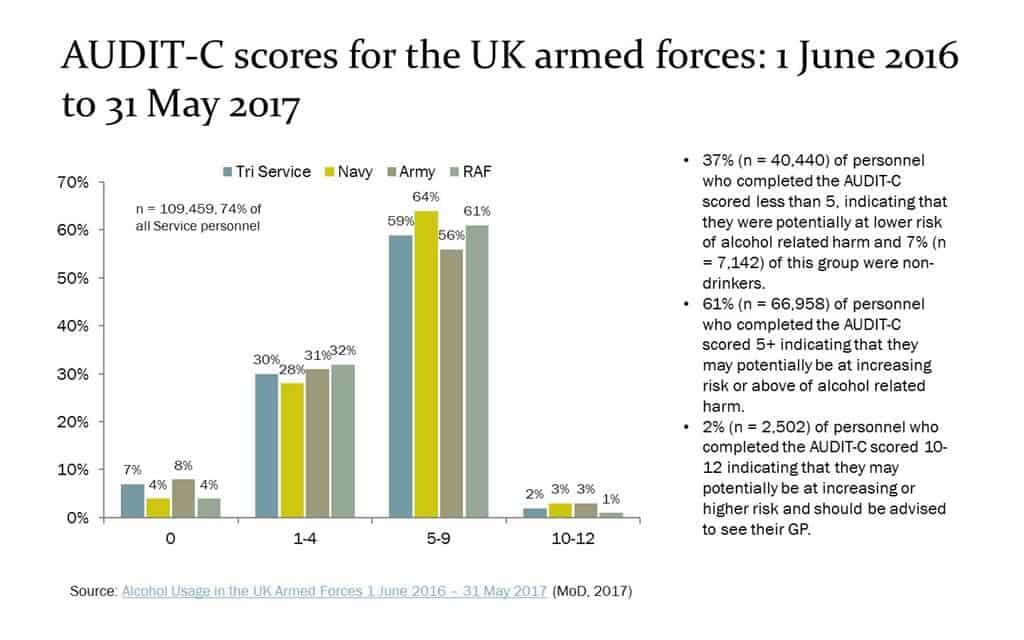 |
source: @andrewbrown365
Of the personnel who scored 1+, 80% (80,662) were given an alcohol advice leaflet. Of the personnel who scored 5–12, 63% (42,074) were given an Alcohol Brief Intervention (ABI). 1% (780) of personnel who scored 5–12 declined the ABI.
White cider linked to premature deaths in Scotland
Data sharply highlights “personal toll linked to heavy alcohol consumption”
A study published by Scottish Health Action on Alcohol Problems (SHAAP) in conjunction with Edinburgh Napier University sheds more light on the harmful impact of alcohol in Scotland’s two major cities.
The findings of ‘Mortality among a cohort of heavy drinkers in Edinburgh & Glasgow’ come from detailed assessment and follow-up of 639 heavy drinkers attending NHS services in Glasgow and Edinburgh. The study shows the extent of early death, with 16% (105) of these patients dying over the subsequent 2½ years at an average age of 51, around 25 years younger than typical life expectancy in Scotland.
The Napier study also shows significant consumption of cheap alcohol – especially cider – by these now deceased patients. Within the Glasgow participants, significant associations were found for being deceased and ‘any drug use’ and being a white cider drinker. For men, significant associations were found for being a deceased participant and consuming mainly white cider and amber cider.
Deceased patients in both cities paid significantly less for their unit of alcohol than surviving patients (a median unit price of 41 pence versus 48 pence in Edinburgh and a median unit price of 38 pence versus 46 pence in Glasgow).
The most common underlying cause of death (46% of cases) was liver conditions, including hepatitis and hepatocarcinoma.
Dr Jan Gill, Associate Professor at Edinburgh Napier University and lead researcher for the report, said: “The data sharply highlight the personal toll linked to heavy alcohol consumption, while the full extent of its earlier impact on each drinker’s quality of life and personal relationships can only be guessed”.
ALCOHOL SNAPSHOT: New analysis reveals sociodemographic predictors of risky alcohol consumption
Decision Tree Model of AUDIT Group 2+ (as a % of all drinkers).
The numbers in brackets show the percentage of respondents in AUDIT category 2,3 or 4 in the respective subgroup
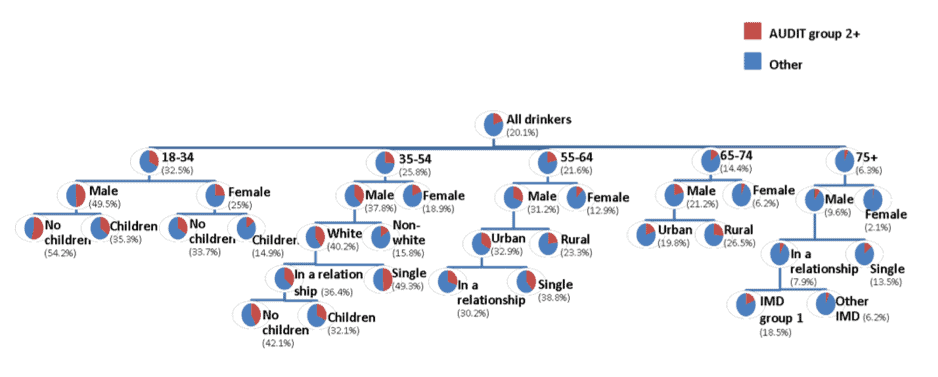
Analysis of a new survey conducted by Public Health England (PHE) reveals the prevalence of heavy drinking among different subgroups, as well as the characteristics most closely associated with different consumption patterns. The chart above represents PHE’s ‘decision tree model’, which predicts the prevalence of being an increasing risk or heavier drinking (i.e. being in Group 2 or higher in the World Health Organization’s Alcohol Use Disorders Identification Test [AUDIT]) based on people’s attributes.
The model suggests that the single best predictor of risky drinking is a person’s age, followed by their gender. However, other factors are only significant predictors for certain subgroups – for example, ethnicity is associated with risky drinking only among 35–54 year olds, while having children is only significant for those under 54. The subgroup with the highest proportion (54%) of increasing risk or higher drinkers is 18–34-year-old childless men. At the other extreme, only 2% of over 75 women drank at risky levels.
Noting that there is a lack of reliable data at a local authority level, PHE commissioned the survey of 9,683 people in 25 local authorities to try to understand geographic variation in alcohol consumption. They found that levels of abstention, binge drinking and risky alcohol use varied significantly between them. However, since it was deemed infeasible to robustly survey every local authority, the decision tree model was built to provide estimates for local authorities beyond the scope of the research.
Podcast
Our monthly podcast features interviews with experts from across the sector.
Gambling industry harms and parallels with the alcohol world
Will Prochaska –
Coalition to End Gambling Ads