In this month’s alert
Editorial – May 2017
Welcome to the May 2017 edition of Alcohol Alert, the Institute of Alcohol Studies newsletter, covering the latest updates on UK alcohol policy matters.
In this month’s issue, a new alcohol availability report compares the alcohol policies of Australian and UK licensing authorities. Other articles include: new official figures on the nation’s health show that alcohol-related admissions continue to rise, breaking 1.1 million for the first time since records began; study finds that the poorest in society are at greater harm from heavy drinking; and another from World Cancer Research Fund finds that just one alcoholic drink a day can increase the risk of contracting breast cancer.
Please click on the article titles to read them. We hope you enjoy this edition.
TOP STORY: UK alcohol laws should look Down Under to tackle crime and disorder
 New report finds ‘Last Drinks’ policies reduce harms associated with late-night drinking (30 May)
New report finds ‘Last Drinks’ policies reduce harms associated with late-night drinking (30 May)
Shorter hours of sale for alcohol could ease the pressure on ambulances, emergency departments, hospitals and the police, suggests a study of licensing laws in Australia and the UK.
This is the key finding from a new report published by the Institute of Alcohol Studies (UK) and the Foundation for Alcohol Research and Education – FARE (Australia).
Anytime, Anyplace, Anywhere? compares and assesses alcohol licensing policies in Australia and the UK and offers a series of recommendations on how to reduce and prevent alcohol-related harm based on shared learnings. This is the first comparative study of alcohol availability policies in these two countries, which share similar drinking cultures.
Fourteen alcohol control policies were rated for their effectiveness in reducing harm and value for money using an ‘alcohol availability scorecard’. Australia’s ‘Last Drinks’ policy, which requires venues to restrict on-premises (pubs, bars and restaurants etc) alcohol sales after a specified time at night or in the early hours of the morning, scored highest. The lowest scoring policies were alcohol industry voluntary schemes and UK Late Night Levies.
Speaking ahead of the launch, Kypros Kypri, Professor of Public Health at University of Newcastle, Australia said: “There is strong evidence to show that earlier closing times can make a significant difference to the strain alcohol places on emergency services. In Sydney, bringing forward closing times to 3am was associated with a 25% reduction in alcohol-related presentations to the local hospital.”
The report offers 10 recommendations for reducing alcohol-related harms through existing licensing policy frameworks. These include:
- Restricting trade hours of on-licence venues to limit the availability of alcohol in the early hours of the morning
- Enhancing community involvement, better facilitating the engagement of local residents with licensing systems
- Adding / prioritising public health and / or harm minimisation objectives in alcohol legislation
- Restricting the sales of high risk products in areas of concern; and
- Deprioritising government support for industry voluntary schemes in place of policies supported by evidence.
Co-presenter Jon Foster, Senior Research and Policy Officer at IAS (see Soundcloud image below, left), said: “Even modest reductions in bar opening times would take the pressure off hard pressed A&E departments, who would undoubtedly welcome a 25% reduction in alcohol-related admissions, as happened in Australia. Legislation should empower licensing authorities to curb excessively late opening times for clubs and bars where these are causing a problem.”
This report follows the publication of an inquiry into the Licensing Act (2003) by a cross-party committee of Lords published earlier this year, which concluded that it is “fundamentally flawed” and in need of “a major overhaul.”
Click on the Soundcloud player below to hear the Alcohol Alert podcast covering the report’s launch, featuring interviews from Kypros Kypri (see image, right) and report co-author Claire Wilkinson (centre).
Alcohol-related admissions continue to rise
Annual report highlights rising admissions and costs of prescriptions (03 May)
There were a record 1.1 million alcohol-related admissions to hospitals in England in 2015/16, according to the latest Statistics on Alcohol England 2017 report.
Published by NHS Digital (formerly the Health Social Care and Information Centre), the report shows that, despite plateauing consumption and death levels, the number of admissions for alcohol-related reasons has risen every year since records began in 2003/04.
The total number of alcohol-related NHS hospital admissions based on primary and secondary diagnoses (broad measure), rose 4% on the previous fiscal year (1,078,810 in 2014/15) and is 78% greater than in 2005/06.
73% of admissions were down to partially attributable conditions, cardiovascular disease being the most common; more than half a million (estimated 556,960) admissions occurred in 2015/16, up 5% on previous year (24,800) and up 130% on a decade ago (315,520).
The total number of alcohol-related NHS hospital admissions in England based on the narrow measure (primary diagnoses and external cause codes in secondary diagnosis fields) also reached a new record level. There were 339,280 alcohol-related hospital admissions of this type in 2015/16, up 3% on the previous year (330,010 in 2014/15) and the third annual increase in a row.
Seven out of every ten admissions were down to partially attributable conditions, cancers being the common type; almost 80,000 took place in England in 2005/06, the highest number since records began.
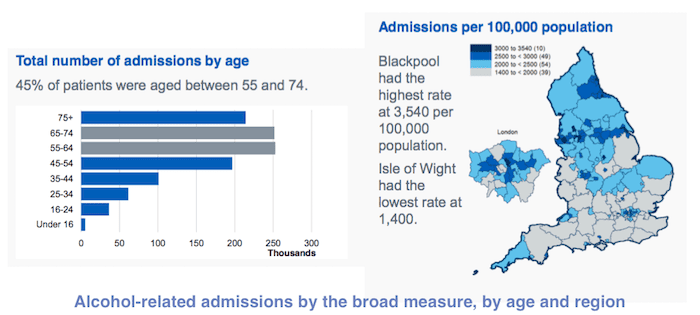
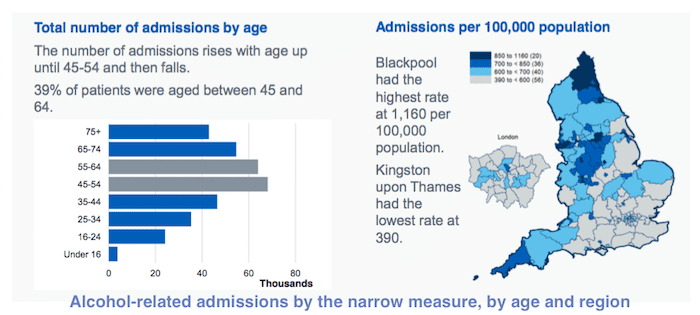
Age and region
In both cases, middle-aged and older people were most likely to present with alcohol-related conditions; 45% of patients admitted to NHS hospitals for alcohol-related conditions by the broad measure were aged between 55 and 74 years of age, and 39% of patients admitted under the narrow measure were aged between 45 and 64 years of age.
Regionally, Blackpool is the capital of alcohol-related hospital admissions, with the (worst) highest rate by both the broad (3,540 per 100,000 population) and narrow measures (1,160 per 100,000 population).
Cost of prescription drugs rises to record high
In 2016, approximately 188,000 prescription items were dispensed for as part of patient alcohol treatment in primary care and NHS hospitals, 4% short of 2015’s record 196,000 dispensations. However, it is 63% higher than a decade ago, and the cost of these drugs has more than doubled since then. Total Net Ingredient Cost (NIC) reached a new record £4.87 million in 2016, 24% higher just 12 months before (£3.93 million). This is solely down to the cost of Disulfiram (marketed as Antabuse / Antabus) doubling in price over the period.
Wider outlook: During habits stay the same
Statistics on Alcohol England 2017 coincided with the release of the Office for National Statistics’ (ONS) Adult drinking habits in Great Britain: 2005 to 2016, which found little change in consumption patterns across the entire Great British Isles. Approximately 29 million people (56.9% of Opinions and Lifestyle Survey respondents) aged 16 years and over drank alcohol in 2016. This small decline on the previous year takes the proportion of adult drinkers in Britain to its lowest level since 2005.
The majority of drinkers kept within the weekly consumption guidelines released last year, but the number of those who exceeded the guidelines on their heaviest drinking day in the week remained the same – nearly 2.5 million adult drinkers consumed more than 14 units on their heaviest drinking day.
Almost 5 million adults (9.6%) were frequent drinkers (drank on 5 or more days in the last week). Of those adults who drank, 26.8% (around 7.8 million people) “binged” on their heaviest drinking day prior to interview.*
This compared with around 10.6 million people in the population who said that they did not drink alcohol, most represented by 16 to 24 year-olds. The ONS found that young people aged 16 to 24 years in Great Britain are less likely to drink than any other age group, but that when they do drink, consumption on their heaviest drinking day tends to be higher than other ages. Less than half (46%) of those aged 16 to 24 years reported drinking alcohol in the previous week, compared with 64.2% of those aged 45 to 64 years.
Despite this, young drinkers are more likely than any other age group to “binge” on their heaviest drinking day. Among drinkers aged 16 to 24 years, 37.3% reported binge drinking on their heaviest drinking day in 2016 compared with just 10.3% of drinkers aged above the age of 65 years.
* The Government’s Alcohol Strategy defines binge drinkers as men who report exceeding eight units of alcohol on their heaviest drinking day in the week before interview, and women who report exceeding six units.
Poorest at greater risk of harm from heavy drinking, study finds
Increased consumption is “disproportionately harmful” to those on lowest incomes (10 May)
Drinking heavily is more harmful to the poorest people in society, who are at greater risk of illness or death because of alcohol consumption, according to a medical study.
Published in medical journal The Lancet Public Health on Wednesday, it found there is a marked link between socio-economic status and the harm caused by drinking alcohol excessively.
Compared with light drinkers in advantaged areas, excessive drinkers were seven times at risk of an increase in alcohol harm. This contrasted with excessive drinkers in deprived areas, who were 11 times at risk of an increase.
Harmful impacts of alcohol are higher in socio-economically disadvantaged communities. However, until now it was unclear whether those were as a result of differences in drinking or as a result of other factors.
Lead author Dr Vittal Katikireddi, of the University of Glasgow, said: “Our study finds that the poorest in society are at greater risk of alcohol’s harmful impacts on health, but this is not because they are drinking more or more often binge drinking.
“Experiencing poverty may impact on health, not only through leading an unhealthy lifestyle but also as a direct consequence of poor material circumstances and psychosocial stresses.
“Poverty may, therefore, reduce resilience to disease, predisposing people to greater health harms of alcohol.”
The authors linked different sets of data to bring together information from Scottish Health Surveys with electronic health records, studying more than 50,000 people. It suggested that even when other factors are accounted for, including smoking and obesity, living in deprived areas was consistently associated with higher alcohol-related harms.
Researchers defined harm from alcohol consumption based on deaths, hospital visits and prescriptions that were attributable to alcohol.
Study co-author Dr Elise Whitley said: “Heavier drinking is associated with greater alcohol-related harm in all individuals.
“However, our study suggests that the harm is greater in those living in poorer areas or who have a lower income, fewer qualifications or a manual occupation.”
Responding to the University of Glasgow study, Professor Sir Ian Gilmore, chair of the Alcohol Health Alliance UK (AHA), said:
“The findings in this study are worrying if not altogether surprising. It is clear that the way alcohol is being sold and promoted in Scotland and elsewhere in the UK is harming some of the most vulnerable people in society.
“On the other hand, we know what needs to be done, in particular to tackle the scourge of cheap alcohol. In real terms, alcohol is 60% cheaper than it was in 1980 and measures like strength based pricing would disproportionately benefit the poorest groups, in terms of reduced deaths, illness and hospital admissions. Studies have shown that 82% of the lives saved through minimum unit pricing would come from the lowest income groups.
“Overall, in the first year alone minimum unit pricing in Scotland is expected to save 60 lives and lead to 1,600 fewer hospital admissions and 3,500 fewer crimes, yet its introduction has been held up for years by alcohol industry legal challenges.
“Importantly, minimum unit pricing would leave pub prices untouched, and moderate drinkers would spend only about £2.25 extra per year with a 50p minimum price.”
Drug and alcohol treatment sector – on borrowed time?
Adapted from Drink and Drugs News (12 May)
The new drug strategy is in limbo. Delayed for months without explanation, the questions are mounting against a backdrop of the highest number of drug-related deaths ever recorded. In the new year, the government said ‘soon’. In February they confirmed ‘shortly’. At the end of April, the parliamentary under-secretary of state at the Home Office, announced: “We are currently developing the new drug strategy, working across government and with key partners. The new strategy will be published in due course.”
But with the general election taking place on 8 June, no-one is expecting progress anytime soon. Furthermore, there is no hint of an alcohol strategy, apart from in Scotland, despite problematic alcohol use affecting many more people than drugs.
At the latest cross-party parliamentary group on drugs, alcohol and justice, Colin Drummond, professor of addiction psychiatry at King’s College London, was invited to speak about alcohol misuse and treatment. He began by outlining the worsening picture on alcohol, stating that “alcohol-related health conditions, including liver disease, have increased and alcohol-related hospital admissions have doubled.” But his talk went on to explore the deepening crisis for the drug and alcohol sector.
“We’ve had a world-class addiction system in the UK, and we’re in danger of losing it. We’re in danger of it not existing in a few years’ time,” he said. Looking at the recent rise in drug-related deaths (DRDs) he referred to the government’s reaction to a previous epidemic around 2001: “In the 2000s we had a huge investment in treatments, so drug deaths began falling. But they’re now at their highest since records began.”
So what’s going wrong? Why are we failing? “Declining resources for this population” were an obvious factor, combined with the disastrous effect of constant retendering. Prof Drummond stated that “people with complex needs are not getting the same access to treatment as before” and went on to say that the “biggest impact of constant retendering is going to be on people with the most complex needs. They’re not attractive people to treat – they’re costly, with poor outcomes.”
Furthermore, when contracts are tendered, the expectation is that the service will see ‘twice the number of people with half the amount of money,’ he said. ‘So they strip staff costs and have fewer qualified staff and more volunteers.’ It was also an extremely expensive process – ‘money that could have been spent on treatment instead of lawyers drawing up contracts’.
With retendering taking place every three years in local authorities, clients were constantly affected by the changeover process. Add to this the loss of specialists to the field – “in addiction psychiatry we’ve lost 60% of training places in England” – and you have the perfect storm, he said. “It looks like there are plenty of people in treatment, but the people in most need are being denied care. If they’re not being taken care of here, they will pop up elsewhere – in A&E, GPs’ surgeries and in prison… there is an artificial separation between health and social care.”
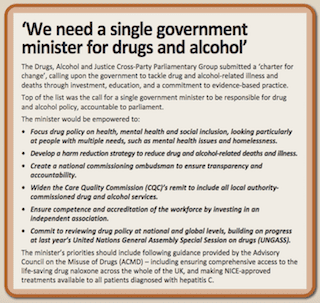
So what needs to change? Prof Drummond suggested immediate recommendations for the incoming government:
- Ring-fence funding that’s going into addiction treatment. “Ring-fencing needs to be safeguarded not further depleted,” said Prof Drummond. “Cutting these services is a false economy. Local authorities will only see it from their perspective, but it will cost them more money in the long term.”
- Bring the NHS back into the fold: “We felt it was wrong to put everything in the control of local authorities.”
- Put a moratorium on retendering. “We see no evidence that it improves services.”
- Protect specialism and experience, eg addiction psychiatry. “No area should fall over for lack of experience.”
- Deal with people with complex needs properly. “We need to rebalance the system to do this – and if we don’t treat them, they cost a lot to the economy.”
- Back minimum unit pricing (MUP). “It would have huge benefits – to both moderate drinkers and to people at the severe end of the spectrum.”
- Increase research capacity. “If we don’t understand the impacts, we won’t learn.”
Discussion between members of the APPG – which includes MPs, treatment providers, specialist and advisory groups and people representing service user and recovery communities – reinforced the need for action.
“A lot of this isn’t new but political will is lacking,” said Alex Boyt, who worked for years in service user involvement. “It’s a lose-lose conversation – people who are not cost-effective are not being treated.” The ‘relentless commissioning’ also exacerbated the situation: “Each time clients are lost, old and new providers blame each other.”
Prof Drummond said that “those most affected by cuts have been rehabs”, to which Caroline Cole, interim chief executive at Broadway Lodge, added: “We’ve had to pull back on the numbers of people with complex needs as the local authority can’t pay us what it costs us to treat them.”
“Why doesn’t the treasury see the madness of the way we’re running things? Why aren’t they looking for a rational approach?’ asked one MP.
“What we’ve done as a group is to approach all the ministers responsible and given them the evidence,” said Lord Ramsbotham, the APPG’s chair.
“They’ve patted us on the head but not reflected the evidence. The cost of not doing one thing in an area is going to be seen in another – all exemplified in the lack of a national drug strategy.”
Loophole closed in underage drinking crackdown
Adapted from Police Professional (15 May)
Giving alcohol to children to drink in public is now an arrestable offence after the Scottish Government tightened the law around underage drinking.
The new law, introduced on as part of the Air Weapons and Licensing (Scotland) Act 2015, closes a loophole that was giving under-18s access to alcohol despite the ban on buying them drinks.
The provision also introduces a ‘fit and proper person test’ to alcohol licensing and requires licensing boards to produce annual income and expenditure reports to improve their accountability and transparency.
Last year (November 2016), MSPs banned Police Scotland from stop searching under-18s for alcohol without legal cause. A government review found under 10% of consensual searches of children found alcohol, which rose to 16.3% for adults.
However, officers can still require underage drinkers to surrender any alcohol they are caught with.
Justice Secretary Michael Matheson said the new measures will “strengthen the range of interventions” available to officers.
“While many young people will not undertake underage drinking, we know that groups of young people drinking outside can be an intimidating sight to members of the public and are often linked with a number of public order offences,” he said.
“Furthermore, underage drinking can cause short and long term harm to health, as well as put young people in dangerous situations when drunk.
“So it is entirely correct that Police Scotland are able to deal effectively with those who supply alcohol to young people.”
Police unit backs new approach to cut alcohol-related crime
From The Scotsman (16 May)
A respected police unit has given its backing to alcohol minimum pricing and called for tougher licensing laws to help tackle violent crime on Scotland’s streets.
The Violence Reduction Unit (VRU) said there is currently an “over provision” of both off-licences and bars in towns and cities.
It called for the police to be given a bigger role in licensing decisions and said those who commit acts of violence under the influence should have their “right to drink” taken away from them.
Now part of Police Scotland, the VRU was initially set up by Strathclyde Police in 2005 and is credited with helping Glasgow shake off its “murder capital of Europe” tag by taking a public health approach to gang-related violence.
Acting director Will Linden said Scotland could not hope to import a “cafe culture” from continental Europe due to long-established problems with alcohol.
He said: “What we’d like to see is a more evidence-based approach to licensing, a move away from just the economic argument of filling up our city centres with both on- and off-sales.
“We’re not calling for closing them down just now but when new licences are considered, they should be considered based on the impact they will have on a community or local area by looking at levels of crime and levels of health and deprivation.
“Years ago people talked about Scotland having a café culture, but if you want that you open up cafés, you don’t open pubs. “You can’t import a European system into Scotland because this is a country which has a very different relationship with alcohol.”
The Scottish Government is currently fighting an attempt by the Scotch Whisky Association to block the introduction minimum pricing, with a hearing due to take place at the Supreme Court in London in July. Mr Linden said that alcohol is involved in about 70% of all violence and up to 60% of all homicides.
He said: “We should be looking at over provision because we already have too many licensed premises in Scotland. This is not about prohibition – alcohol is part of our culture – but we need a sensible debate.”
A Scottish Government spokesperson said: “Our Framework for Action outlines a package of more than 40 measures to reduce alcohol-related harm in Scotland. These include licensing measures like minimum unit alcohol pricing, the quantity discount ban, a ban on irresponsible promotions as well as a lower drink drive limit, improved substance misuse education, and our nationwide alcohol brief intervention programme.”
An open letter to ministers on the AudioVisual Media Services Directive (AVMSD)
An open letter to ministers (22 May)
On 22 May 2017, 17 public health organisations wrote an open letter to the Health Ministers of all European Union Member States in light of the meeting of the European Council on Education, Youth, Culture and Sports.
The full text is below.
******
Dear Ministers,
The signatories to this letter would like to present suggestions to the ongoing negotiations on the Audiovisual Media Services Directive (AVMSD), relating to commercial communications.
Obesity and alcohol consumption are major causes of preventable ill-health and early death.
Currently, over half of EU citizens are overweight or obese and Europe’s prevalence rate for children’s (aged 5 to 17) obesity is greater than 30%. Becoming obese earlier in life clearly amplifies certain health risks.
Europe is also the heaviest drinking region in the world, with high alcohol use among adolescents. On average, four in five students (aged 15 to 16) report lifetime alcohol experience and every second student reported alcohol use in the last 30 days.
These consumption patterns amplify certain health risks which pose a burden on the sustainability of health systems.
It is well-established that advertising causes both early onset and changes in consumption patterns, favouring the products advertised.
Nevertheless, children and young people in Europe are still subjected to the aggressive marketing of alcohol and foods high in fat, sugar and salt (HFSS) on a frequent basis.
The ongoing revision of the Audiovisual Media Services Directive (AVMSD) presents a key opportunity to reduce exposure of Europe’s children to commercial communications for products that can harm their health (health-harmful products) – it is an opportunity that should not be missed by EU governments.
We note that there are some positive aspects in the European Commission’s proposal – for example, recognition of exposure as problematic. However, it relies on weak policy measures, such as self-regulation, and fails to provide effective protection of children from commercial communications.
The European Parliament’s position, as adopted by its lead committee, weakens the commission’s proposal, and we are greatly concerned that the EU institutions will fail to grasp this once-in-a-decade opportunity to protect children from commercial communications of health-harmful products.
Minimising exposure
We identified three improvements to the EU commission’s proposal for AVMSD – to better achieve the objective of the AVMSD and to minimise children’s exposure to HFSS food and alcohol marketing:
- Minimise children’s exposure to the marketing of health-harmful products:
Mandatory measures are needed to minimise the exposure of children to health-harmful marketing, regardless of whether the advertising is directly aimed at them or not.
Measures should cover television, on-demand services and online video-sharing platforms and include a mandatory provision for member states to determine and implement a watershed that adequately captures children’s and adolescents’ viewing times depending on the country.
Self-regulation and voluntary commitments without a regulatory framework have, to date, failed to achieve meaningful reductions in exposure. We strongly recommend that you keep a reference to the World Health Organization’s (WHO’s) nutrient profile model as a means of defining HFSS foods.
- Exclude alcohol and HFSS food from product placement and sponsorship:
Product placement and sponsorship of alcoholic beverages and HFSS food are effective marketing techniques, and should be prohibited alongside tobacco and medicinal products – and not just from children’s programmes or those with a significant children’s audience.
- Ensure that Member States can effectively limit broadcasts from other countries on public health grounds:
The efforts of front-runner governments to reduce the negative health effects of alcohol and HFSS food marketing must not be undermined by broadcasters established in other EU member states. The European Commission’s proposal to this effect should be supported.
We hope to work constructively with you to develop a final text of the revised AVMSD that more effectively protects children and adolescents from commercial communications of health-harmful products.
Yours sincerely,
With kind regards.
******
The signatories are:
Alcohol Policy Youth Network (APYN),
European Association for Study of the Liver (EASL),
European Centre for Monitoring Alcohol Marketing (EUCAM),
European Heart Network (EHN),
European Public Health Alliance (EPHA),
IOGT International,
International Association of Mutual Benefit Societies (AIM),
Standing Committee of European Doctors (CPME),
United European Gastroenterologist (UEG),
Alcohol Action Ireland (AAI),
British Medical Association (BMA),
Cancer Research UK,
IOGT- NTO,
Institute of Alcohol Studies (IAS),
Scottish Health Action on Alcohol Problems (SHAAP),
STAP,
European Alcohol Policy Alliance (Eurocare).
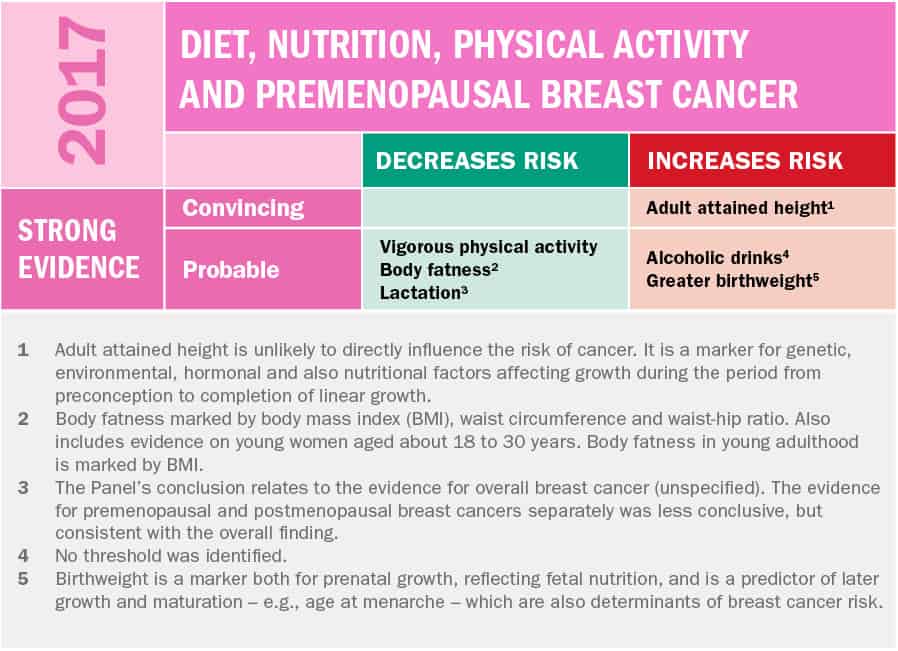
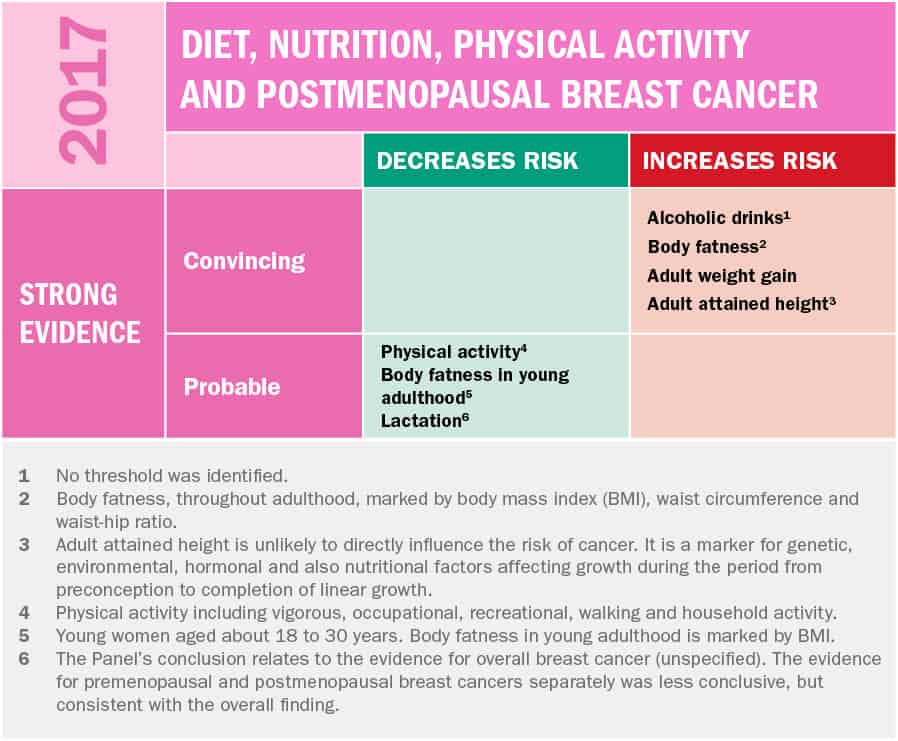
Just one alcoholic drink a day can increase breast cancer risk
Report from cancer charity finds raised risk pre- and post-menopause (23 May)
Drinking just one alcoholic drink a day can increase breast cancer risk, a new report by the World Cancer Research Fund has revealed.
The latest Continuous Update Project – providing new data for the breast cancer section of our 2007 Second Expert Report and the 2010 CUP Breast Cancer Report – analysed 119 studies and included data on 12 million women and 260,000 cases of breast cancer, and found “strong evidence” that drinking just the equivalent of a small glass of wine or half a pint of beer a day (about 10g alcohol content), could increase your pre-menopausal breast cancer risk by 5% and your post-menopausal breast cancer risk by 9%.
Dr Rachel Thompson, Head of Research Interpretation at World Cancer Research Fund, said: “To help prevent breast cancer, one of the most important steps women can take is to not drink alcohol or reduce the amount of alcohol they drink.
“Maintaining a healthy weight and getting enough exercise are also important for preventing breast cancer.
“It may be the most common cancer in women worldwide, but our evidence shows that there are steps that women can take to significantly reduce their breast cancer risk.”
Breast cancer is the most common cancer in women in the UK with over 55,000 new cases each year. It is responsible for more than half a million deaths worldwide each year. World Cancer Research Fund estimates that about 12,000 cases of breast cancer could be prevented in the UK each year if nobody drank alcohol.
The UK government recommends drinking no more than 14 units a week equivalent to 7 drinks a week, spread across at least 3 days.
Professor Sir Ian Gilmore, Chair of the Alcohol Health Alliance UK (AHA) said: “Only 1 in 10 people are aware of the link between alcohol and cancer, and with the evidence on breast cancer and alcohol being so strong, it is vital that consumers are aware of this fact.
“People have a right to know about the risks associated with alcohol, which is why the AHA is calling for specific health warnings on alcohol labels and sustained, government-backed campaigns warning people of the risks. In addition, policymakers should take action to reduce the overall amount of alcohol people drink, which would reduce the burden of breast cancer in the UK. Price-based measures, such as minimum unit pricing, would be the most effective at doing this.”
The Continuous Update Project is an ongoing programme to analyse global research on how diet, nutrition, physical activity and weight affect cancer risk and survival. Among experts worldwide it is a trusted, authoritative scientific resource, which underpins current guidelines and policy for cancer prevention.
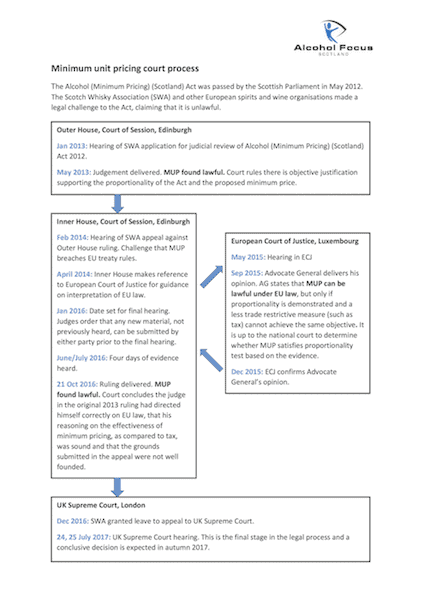
Minimum unit pricing, 5 years on
Where are we now with the controversial alcohol pricing policy? (24 May)
Five years ago this month, the Scottish Parliament successfully passed legislation stating that ‘Alcohol must not be sold … at a price below its minimum price’ (Section 6A(1) of the 2005 Act as amended), set at 50 pence per unit.
Yet, the Alcohol (Minimum Pricing) (Scotland) Act 2012 has still not been implemented, as it is subject to a court challenge from the Scotch Whisky Association and a number of other wine and spirit industry bodies (the Associations), write Graeme Young and Fiona Carter for legal firm CMS Cameron McKenna in Lexology.
The SWA et al argued that MUP has an effect equivalent to a quantitative restriction on importing goods and is therefore contrary to the European Union principle of the free movement of goods, focusing specifically on Article 34 of the Treaty on the Functioning of the EU (TFEU).
And although the issue has been taken to the highest European Court and back, judges presiding over the case at the Houses of the Court of Session found that MUP was a measure compatible with EU law under the legitimate aim of protecting human health, satisfying the derogation provided for in Article 36 TFEU.
On the anniversary of the policy’s introduction, and as a final verdict is about to be passed on its legality this summer, alcohol campaigning charity Alcohol Focus Scotland has depicted the sequence of events in a handy diagram (see below).
Open letter to the candidates for Director General of WHO: UPDATE
Open letter to the candidates for Director General of WHO: UPDATE (30 May)
In April, the Institute of Alcohol Studies, together with partners including the World Obesity Federation, International Baby Food Action Network, UK Health Forum and Center for Health Science and Law issued an open letter to the three remaining candidates for the position as Director General at the WHO. The letter was signed by 64 international and national NGOs, and published in The Lancet on 27 April 2017 (the letter can be read in full here).
The letter invited each candidate to present their thoughts on the issue, focusing on the need for a WHO free of commercial influence that protect public health in the best possible way:
‘Alcohol, food, pharmaceutical, and medical technology industries should comply with policies developed by WHO and its Member States. Their role is not in public health policy formulation, risk assessments, risk management, or priority setting, nor in determining normative quality standards and legally binding regulations to protect and promote public health. These processes must be undertaken in an environment free of commercial influence’.
Since its publication, more names have been added to the list of signatories since its publication (see updated list here), while two of the three candidates issued their responses to the letter: Dr Nabarro (UK) and Dr Nishtar (Pakistan).
The new Director General was elected at the 70th World Health Assembly in Geneva, Switzerland, held 22 – 31 May 2017. Dr Tedros Adhanom Ghebreyesus was elected to succeed Dr Margaret Chan, commencing 1 July 2017.
Podcast
Our monthly podcast features interviews with experts from across the sector.
Gambling industry harms and parallels with the alcohol world
Will Prochaska –
Coalition to End Gambling Ads