In this month’s alert
Editorial – November 2014
Welcome to the November edition of Alcohol Alert, the Institute of Alcohol Studies newsletter, covering the latest updates on UK alcohol policy matters. In this issue, acclaimed public health expert Professor Sir Michael Marmot gives his thoughts on our new report “Alcohol, health inequalities and the harm paradox“, which asks why lower socioeconomic groups experience greater health problems due to alcohol despite drinking less than those on higher incomes. Other articles include: Stark north-south divide over admissions and mortality rates for alcoholic liver disease, approval of a controversial new drug for treating alcohol dependence; and remembering 50 years of THINK! drink-drive campaigns.
Please click on the article titles to read them. We hope you enjoy this edition.
Alcohol, drugs and tobaco joint strategic needs assessment support pack
Public Health England’s alcohol, drugs and tobacco division has published a joint strategic needs assessment (JSNA) support pack to help local areas develop joint strategic needs assessments and local joint health and wellbeing strategies that effectively address public health issues relating to alcohol, drug and tobacco use.
The support pack, which is now in its third year, is reviewed and updated annually, consists of 8 resources covering young people’s substance misuse and adult alcohol, drug and, for the first time in 2014, tobacco use.
For each topic area there are good practice evidence-based prompts to support local areas to assess need, plan and commission effective services and interventions. The second component for each topic is a bespoke data pack for every local authority to support needs assessment and commissioning.
Joint Review – Public Health England and the Association of Directors of Public Health
October 3, 2014 in ADPH Updates, Alcohol and Drugs, Uncategorized by Georgina Morgan
This joint review of drug & alcohol commissioning by local authorities in England was published on 3rd October 2014 along with a covering letter from PHE Chief Executive Duncan Selbie and ADPH President Dr Janet Atherton.
This followed a snapshot review of commissioning across local authorities in England to identify where there have been changes to commissioning and its impact on outcomes, as well as future plans for commissioning.
In welcoming publication of the report, ADPH President Dr Janet Atherton commended this collaborative approach, which will serve as a strong basis for continuing sector-led improvement of substance misuse services and result in improved outcomes for local populations. Janet acknowledged the sterling work undertaken by PHE colleagues and ADPH members in support of the Review, and thanked all those who had contributed to the review process.
Scotland: Number of licensed premises linked to alcohol-related illness and deaths
Neighbourhoods in Scotland with the most licensed premises have alcohol-related death rates more than double those in neighbourhoods with the fewest.This is the main conclusion of a new study presented at Alcohol Focus Scotland’s national licensing conference.
The study, commissioned by Alcohol Focus Scotland and undertaken by researchers at the Universities of Edinburgh and Glasgow, investigated the links between alcohol outlet availability and health outcomes across the whole of Scotland.
The researchers used Scottish ‘datazones’ – 6,505 small areas representing neighbourhoods. They compared the number of alcohol outlets within each neighbourhood with records of alcohol-related hospitalisations and deaths there. The alcohol-related causes of illness and death included liver disease and alcohol poisoning.
The key findings are:
- Alcohol-related death and hospital admission rates were significantly higher in neighbourhoods with higher numbers of alcohol outlets
- Neighbourhoods with the most alcohol outlets had alcohol-related death rates more than double those in neighbourhoods with the fewest outlets. There were 34 alcohol-related deaths per 100,000 people in neighbourhoods with the most off-sales outlets, compared with 13 per 100,000 in neighbourhoods with the fewest outlets
- Each increase in outlet availability was associated with a higher alcohol-related death rate
- The researchers suggest that off-sales outlets have the greatest potential for alcohol-related harm
Dr Elizabeth Richardson, Centre for Research on Environment, Society and Health at the University of Edinburgh said:
“The role of local neighbourhood environments in enabling drinking has received little attention in Scotland to date, but our findings show that this is a serious oversight. The strong relationship we found between alcohol outlets and related health outcomes leads us to suggest that reducing outlet numbers, particularly in the highest availability neighbourhoods, could have health benefits for the Scottish population.”
Dr Evelyn Gillan, Chief Executive of Alcohol Focus Scotland said:
“This study should encourage all of us to think about how the environment we live in can have a bearing on health. If we want fewer people to end up in hospital or lose their lives because of alcohol, then we have to be concerned about the high number of alcohol outlets in our neighbourhoods. Licensing boards have a key role to play in regulating the overall availability of licensed premises and their decisions should be informed by studies such as this.”
Controversy over new drug to treat alcohol dependence
A drug that can help people who are dependent on alcohol to cut down on the amount they drink, has been recommended in final draft Guidance by the National Institute for Health and Care Excellence (NICE). Dr Marsha Morgan, a scientific adviser to the Institute of Alcohol Studies, was a member of the Evidence Review Group for this Guidance.
The drug, nalmefene, was granted a European marketing authorisation in February 2013, although that decision was criticised by some clinicians on the grounds that there were insufficient data to support the treatment.
The move to licence the drug in the UK has also proved controversial, dividing opinion among addiction experts, with some hailing the drug as a useful weapon in the armoury against alcohol problems, while others attacked the move as an attempt to medicate away what is, in reality, a societal problem.
Joint Review –Nalmefene
In its draft guidance, NICE says nalmefene should be available as an option for the mildly alcohol dependent, a criterion which excludes those with physical withdrawal symptoms, or who require immediate detoxification.The drug is intended to assist those who have sought help to reduce their drinking, and the marketing authorisation states that nalmefene should only be prescribed in conjunction with continuous psychosocial support focused on treatment adherence and reducing alcohol consumption. A course should only be started in patients who continue to have a high drinking risk level 2 weeks after initial assessment.A high drinking risk level is defined as at or above 60 g per day of pure alcohol for men and 40 g per day for women.This translates into an average daily consumption of 7.5 units of alcohol for men and 5 units for women. On the basis of these criteria, nearly 600,000 people will be eligible to receive the treatment.
Nalmefene (also called Selincro and manufactured by Lundbeck) is an opioid receptor modulator taken as a tablet once a day on an as-needed basis and reduces the urge to drink. It is priced at £84.84 for a pack of 28 tablets. The drug is licensed for use alongside psycho-social support to help people reduce their alcohol consumption and give them the encouragement they need to continue with their treatment.
Professor Carole Longson, NICE Health Technology Evaluation Centre Director, said: “Alcohol dependence is a serious issue for many people. Those who could be prescribed nalmefene have already taken the first big steps by visiting their doctor, engaging with support services and taking part in therapy programmes. We are pleased to be able to recommend the use of namelfene to support people further in their efforts to fight alcohol dependence. When used alongside psycho-social support nalmefene is clinically and cost effective for the NHS compared with psychosocial support alone.”
For Alcohol Concern, Chief Executive, Jackie Ballard, said: “It is important that there is a variety of treatments available to support people who want help with their alcohol dependency.
“The introduction of nalmefene will be a useful addition to the clinician’s toolbox, when used in conjunction with other treatment methods to tackle the harmful consequences of alcohol misuse.”
Andrew Langford, Chief Executive of the British Liver Trust, agreed. He said:
“The range of people who put themselves at risk through their drinking is quite wide. Some have not yet experienced social problems and are functioning well until they develop an alcohol-related physical illness such as high blood pressure, cancer or liver disease; while others lose their social supports and then tend to fit the stereotype of the ‘alcoholic’.
Professor Jonathan Chick, a consultant psychiatrist and Honorary Professor at Queen Margaret University Hospital, Edinburgh, said: “The decision by NICE to recommend nalmefene for appropriate patients is important. Although, for many people dependent on alcohol, abstinence is the preferred and optimal goal, nalmefene represents an alternative step, helping people to cut down drinking to less harmful levels when they are not ready and have no medical need to give up alcohol altogether. This may help us to engage many alcohol dependent patients that we know are not currently receiving help.”
Joint Review –The critics
Professor Mark Bellis, alcohol lead for the Faculty of Public Health, said there were relatively simple alternatives that would reduce alcohol consumption without the need “to medicate the middle classes”, such as reducing advertising of alcohol and introducing a minimum price per unit.
He said: “Once again this is going to increase pressure on the NHS when there are alternatives that would reduce pressure on health services by cutting alcohol consumption.
“There are plenty of ways that don’t require prescribing, and the additional pressures on the NHS, that could reduce harmful drinking.
“We need to think very carefully about how we use limited resources and prescribe for people who, with relatively simple population interventions, such as reducing advertising and minimum unit price, could quite easily reduce alcohol consumption to safer levels.”
He added that nalmefene reduced alcohol consumption by a relatively modest amount when compared with counselling alone and added that medicating people always came with the risks of side effects. He also said that it was not known whether the reduction in drinking was maintained long-term.
Dr Niamh Fitzgerald, a lecturer in Alcohol Studies, Institute for Social Marketing (ISM) at the School of Health Sciences, University of Stirling, said:
“The fact that alcohol problems are widespread in society is an important principle for effective policy options such as minimum unit pricing and restrictions on marketing of alcohol.
“It would be unfortunate if the availability of nalmefene led to a sense that the appropriate response to these widespread problems was for the NHS to medicate large numbers of people, rather than initiating these other more effective and less costly approaches to reduce consumption.”
Public support for Leicester street drinking ban
CHECK ON 16 NOVEMBER
Hundreds of people across Leicester have backed plans for a city-wide ban on anti-social public drinking.
A series of public consultations took place across the summer asking whether people supported plans for the police to have stronger powers to tackle problem street drinking linked to antisocial behaviour.
Government legislation, known as Public Spaces Protection Orders, or PSPOs, gives police and police community support officers the power to tackle a wide range of antisocial behaviour problems linked to noise, alcohol and nuisance dogs.
Some controls on street drinking already exist in parts of the city centre, but the latest proposals would see those powers extended to cover the entire city under a PSPO.
In all, 630 people from the across the city took part in the public consultations. Of those, 87% said street drinking was a problem in the city, and 77% of people backed plans to bring in a city-wide ban.
Leicester City Council will now take the results of the consultation to the next meeting of the full council, on November 13, for a decision to be made.
Along with residents’ views, the consultations in Leicester also took into account information from city wardens, parks services, play services, cleansing teams and police neighbourhood officers.
About 73% of people reported noise linked to street drinking as a problem, 70% complained about littering, while 53% said verbal abuse linked to street drinking was an issue.
Other problems linked to antisocial street drinking included intimidation, urination and vomiting, racism, begging and smashing glass.
Assistant City Mayor for neighbourhood services, Cllr Sarah Russell, said: “A very high number of people who took part in these consultations – 87% – felt that street drinking and associated antisocial behavior were real problems for them, and 77% of people supported the idea of city-wide powers to tackle the issue.
“People have told us that they’re suffering with the noise, littering, intimidation, verbal abuse and other unpleasant behaviour linked to street drinking, and this PSPO will give the police greater powers to take action.”
The PSPO would cover anywhere within the city boundary, meaning it can be used to tackle drinking-related antisocial behaviour anywhere where problems are reported.
Officers can order people drinking in these areas to stop, hand over any alcohol or dispose of the alcohol, with people who fail to do so facing a spot fine of up to £100, or up to £1,000 if the case goes to court.
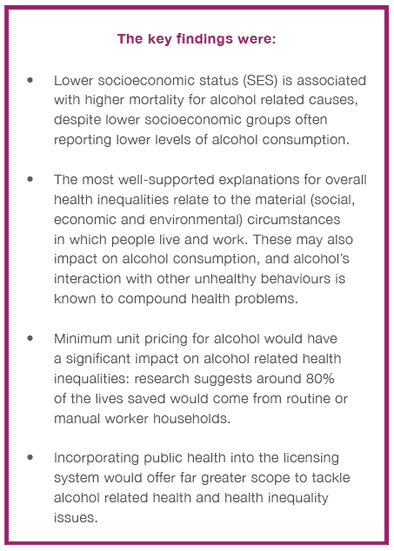
IAS report finds public health measures can help solve alcohol harm paradox
A new IAS report backs calls for tougher alcohol policies – including the introduction of a minimum unit price for alcohol and a public health licensing objective – to help tackle health inequalities in the UK.
 Drawing on international evidence looking into alcohol and health inequalities, Alcohol, health inequalities and the harm paradox attempts to explain why lower socioeconomic groups experience greater health problems due to alcohol, despite drinking less than those on higher incomes.
Drawing on international evidence looking into alcohol and health inequalities, Alcohol, health inequalities and the harm paradox attempts to explain why lower socioeconomic groups experience greater health problems due to alcohol, despite drinking less than those on higher incomes.
The report highlights the findings of a prominent study which shows that in England, alcohol-related mortality is 1.5 – 2 times higher than average within lower socioeconomic groups, and that the most deprived 20 per cent of local authorities have alcohol-specific mortality rates 5.5 times the rate of the least deprived.
It also finds that wider social, economic, cultural and environmental factors relating to overall health inequalities also appear to influence the differences in alcohol consumption and harm outcomes among different socioeconomic groups, leading some researchers to suggest that alcohol is part of a complex system of interactions with other ‘poly-behaviours’. For example, studies have discovered a “supra-additive interaction” between obesity and alcohol consumption, and that a combination of smoking and drinking accelerates the risk of cancer, with tobacco and alcohol-related cancers in the UK 2 – 3 times more common in areas of the most deprivation than the least.
So far, the Public Health Outcomes Framework includes a commitment to ‘reduce differences in life expectancy and healthy life expectancy between communities’ but there are no specific targets or indicators attached to this commitment, despite the fact that alcohol is seen as a contributing factor for almost half of all indicators set within the framework. However, the report also finds much support for specific policies aimed at solving this problem.
One notable example is the minimum unit pricing of alcohol, which has been demonstrated by the University of Sheffield modelling to have a greater impact on harmful drinkers of a lower socioeconomic status (SES). They estimate that a 45p minimum unit price would lead to 860 fewer deaths and 29,900 fewer hospital admissions due to alcohol per year, and that routine or manual worker households – which represent around two-fifths of the UK population – would account for around 80 per cent of these reductions.
The report also found significant evidence highlighting a strong association between social deprivation and alcohol outlet density, with the likelihood of increased consumption potentially resulting in disproportionately more alcohol-related harm in deprived neighbourhoods. This has, in turn, led to a number of groups – including the Local Government Association – to call for the addition of a public health licensing objective so that local authorities can better implement their public health responsibilities.
Commenting on the report, Professor Sir Michael Marmot described how alcohol related health inequalities had been an “issue of great concern” to him for a number of years and that alcohol had the effect of making vulnerable people even more vulnerable. He said:
“People of lower socioeconomic position are more vulnerable to the effects of alcohol, perhaps because of poor nutrition or less resilience in other ways. Some of that could be psychosocial – it could be the obvious thing of who you hang out with would be associated with alcohol-associated violence… It’s a mixture of alcohol and other things that make individuals and groups more vulnerable to the effects of alcohol… given that people of low socioeconomic position are vulnerable to a whole range of different disorders, the report suggests that alcohol interacts with this vulnerability.”
You can hear Sir Michael Marmot give his views on the IAS report ‘Alcohol, health inequalities and the harm paradox‘ by following our Soundcloud link.
Stark north-south divide over admissions and mortality rates for alcoholic liver disease
Public Health England has launched Liver Disease Profiles data revealing significant variations in liver disease morbidity and mortality across the country.
Liver disease is one of the leading causes of premature mortality in England. It is the only major cause of mortality and morbidity which is on the increase, whilst it is decreasing in the rest of Europe.
Over 90 per cent of liver disease is due to three main preventable and treatable risk factors: alcohol, hepatitis B and C, and obesity. Alcohol alone accounts for 37 per cent of liver disease deaths.
Comparisons between county and unitary authorities expose a stark north-south divide in both the hospital admissions and death rates for alcoholic liver disease per 100,000 population. This is best demonstrated when comparing the five lowest admissions rates for alcoholic liver disease along with the five highest rates in the country (see Figure 1 below).
Figure 1: Hospital admission rate for alcoholic liver disease, England, 2012/13
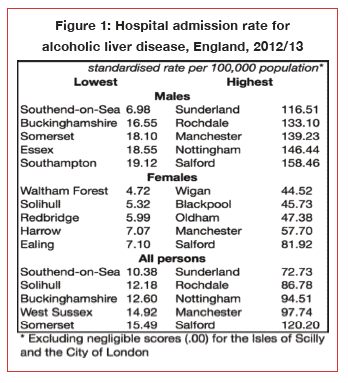
Figure 1 shows that the
lowest hospital admissions rates for alcoholic liver disease are almost
entirely situated in the south of England, whereas the highest rates are predominately
based in the north-west, although Sunderland (72.73/100,000) in the north-east
has the single highest admissions rate for alcoholic liver disease in the
entire country.
There are also pronounced differences between regions over mortality rates from alcoholic liver disease (see Figure 2 below).
Figure 2: Under 75 mortality rate from alcoholic liver disease, England, 2010-12
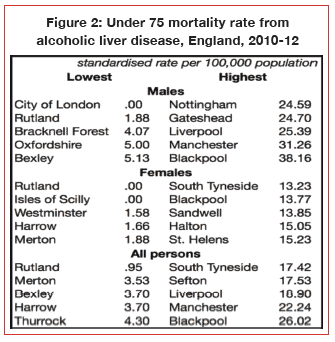
Figure 2 tells a similar
tale; between 2010 and 2012, the lowest rate of deaths from alcoholic liver
disease occurred mainly in the southern parts of the country extending only as
far north as Oxfordshire and Rutland in Leicestershire. In contrast, the
highest rate of deaths from alcoholic liver disease were mainly located in
north-west and north-east regions of the country, stretching only as far south
as the Midlands (Nottingham and Sandwell).
Professor Julia Verne, Lead for Liver Disease at Public Health England, said: “Liver disease is a public health priority because young lives are being needlessly lost. We must do more to raise awareness, nationally and locally, and this is why it is so important for the public and health professionals to understand their local picture.”
Public Health England prioritizes alcohol
Reducing harmful drinking is one of the seven priorities for the next five years announced by Public Health England (PHE), the Government’s lead health promotion agency for England.
The other priorities are tackling obesity, reducing smoking, ensuring every child has the best start in life, reducing dementia risk, tackling antimicrobial resistance, and reducing tuberculosis.
The publication, From evidence into action: opportunities to protect and improve the nation’s health, addresses PHE’s role in helping to bring about change to tackle ‘an epidemic of largely preventable long-term diseases’ amid a growing burden on the present and future NHS.
PHE says it has ‘looked to the evidence to identify where we should focus our efforts’, which involves both promoting healthier behaviours and mobilising support for broader action on improving the public’s health.
In regard to alcohol, the document summarises the challenge by reiterating that alcohol is the leading risk factor for preventable death in 15 – 49 year-olds, and that nine million adults now drink at levels that increase the risk of harm, of whom, 1.6 million show signs of alcohol dependence. It adds that, from 2001 – 2012, the number of people who died due to liver disease in England rose from 7,841 to 10,948 – a 40 per cent increase and in contrast to other major causes of disease that have been declining.
In relation to what it proposes to do about this challenge, PHE says over the next 18 months it will: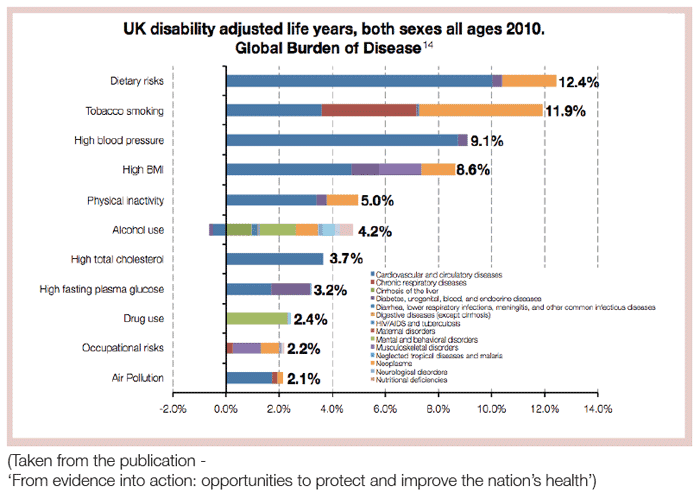
- use alcohol as the trailblazer for a new whole system approach that establishes what works and is clear on the return on investment, enabling Government, local authorities and the NHS to invest with confidence in evidence based policies, prevention and treatment interventions
- produce an independent report for Government on the public health impacts of alcohol and on evidence-based solutions
- produce a framework on liver disease outlining public health actions to tackle liver disease, including alcohol
- expand the Longer Lives web tool to include indicators on alcohol treatment and recovery, and to identify variations in performance
- launch Liver Disease Profiles to support local authority health and wellbeing boards to understand liver disease and its risk factors in their area and, in turn, design effective local population level interventions
- continue to set out the evidence base for the introduction of a minimum unit price for alcohol
- consider the evidence for the inclusion of health as a licensing objective
The last two of these actions necessarily place PHE at loggerheads to some degree with the Westminster Government, which has so far declined to introduce either Minimum Unit Pricing (MUP) of alcohol or a new health objective into the Licensing Act. The public health community will be particularly interested to see PHE’s conclusions in relation to evidence-based solutions to the public health impacts of alcohol, and especially to the issue of alcohol affordability. As well as declining to introduce MUP, the Government has abolished the alcohol duty escalator, presumably intended to increase the affordability of alcohol rather than reducing it, the policy which the scientific evidence suggests is the central plank of any effective strategy to reduce alcohol harm.
In addition to the actions taken by PHE, the Chief Medical Officers are also reviewing the scientific basis of the alcohol advice guidelines, and it is hoped that new draft guidelines will be put out for consultation by summer 2015.
Scotland: Number of licensed premises linked to alcohol-related illness and deaths
Neighbourhoods in Scotland with the most licensed premises have alcohol-related death rates more than double those in neighbourhoods with the fewest.
 This is the main conclusion of a new study presented at Alcohol Focus Scotland’s National Licensing Conference.
This is the main conclusion of a new study presented at Alcohol Focus Scotland’s National Licensing Conference.
The study, commissioned by Alcohol Focus Scotland and undertaken by researchers at the Universities of Edinburgh and Glasgow, investigated the links between alcohol outlet availability and health outcomes across the whole of Scotland.
The researchers used Scottish ‘datazones’ – 6,505 small areas representing neighbourhoods. They compared the number of alcohol outlets within each neighbourhood with records of alcohol-related hospitalisations and deaths there. The alcohol-related causes of illness and death included liver disease and alcohol poisoning.
The key findings are:
- Alcohol-related death and hospital admission rates were significantly higher in neighbourhoods with higher numbers of alcohol outlets.
- Neighbourhoods with the most alcohol outlets had alcohol-related death rates more than double those in neighbourhoods with the fewest outlets. There were 34 alcohol-related deaths per 100,000 people in neighbourhoods with the most off-sales outlets, compared with 13 per 100,000 in neighbourhoods with the fewest outlets.
- Each increase in outlet availability was associated with a higher alcohol-related death rate.
- The researchers suggest that off-sales outlets have the greatest potential for alcohol-related harm.
Dr Elizabeth Richardson, Centre for Research on Environment, Society and Health at the University of Edinburgh, said:
“The role of local neighbourhood environments in enabling drinking has received little attention in Scotland to date, but our findings show that this is a serious oversight. The strong relationship we found between alcohol outlets and related health outcomes leads us to suggest that reducing outlet numbers, particularly in the highest availability neighbourhoods, could have health benefits for the Scottish population.”
Dr Evelyn Gillan, Chief Executive of Alcohol Focus Scotland, said:
“This study should encourage all of us to think about how the environment we live in can have a bearing on health. If we want fewer people to end up in hospital or lose their lives because of alcohol, then we have to be concerned about the high number of alcohol outlets in our neighbourhoods. Licensing boards have a key role to play in regulating the overall availability of licensed premises and their decisions should be informed by studies such as this.”
£25 million to help over-fifties avoid alcohol harm
The Big Lottery Fund is investing £25 million into an alcohol-related harm prevention and awareness programme for the over fifties, in partnership with support charity Addaction.
![]() Rethink Good Health is a UK-wide programme aimed at those aged 50 and over, an age group that Addaction says can find themselves drinking more for a variety of reasons, such as retirement or an increasing problem of loneliness and isolation, as the recent study from the International Longevity Centre and the charity, Independent Age, showed.
Rethink Good Health is a UK-wide programme aimed at those aged 50 and over, an age group that Addaction says can find themselves drinking more for a variety of reasons, such as retirement or an increasing problem of loneliness and isolation, as the recent study from the International Longevity Centre and the charity, Independent Age, showed.
Other findings have also informed the decision. The most recent data from the Office for National Statistics (ONS) shows  that alcohol-related deaths are highest among men aged 60 to 64 years (42.6 deaths per 100,000 population) and women aged 55 to 59 years (22.2 deaths per 100,000). The 2010 General Lifestyle Survey revealed that 20 per cent of people aged 50 and over drink every day compared to 3 per cent of 20 to 24 year-olds.
that alcohol-related deaths are highest among men aged 60 to 64 years (42.6 deaths per 100,000 population) and women aged 55 to 59 years (22.2 deaths per 100,000). The 2010 General Lifestyle Survey revealed that 20 per cent of people aged 50 and over drink every day compared to 3 per cent of 20 to 24 year-olds.
The seven-year Rethink Good Health programme will support a variety of projects, with flagship work taking place in Glasgow, Sheffield, Devon, South Wales and Northern Ireland. In the long term, the programme will help inform policy and practice about preventing alcohol-related harm in later life, improve health and wellbeing of people aged 50 and over who are at risk of developing alcohol problems and help build more effective services aimed at alcohol-related issues.
Peter Ainsworth, Big Lottery Fund Chair, said: “The last thing we want to do is to tell older people they can’t enjoy a relaxing drink with friends and family. With a lot of the current alcohol programmes geared towards younger people, we simply want to make sure that those over 50 are not neglected, are informed about the warning signs around alcohol problems and are able to find help if they need it.
“Addaction will bring their wealth of knowledge and experience into leading Rethink Good Health, along with their partners across the UK, as we aim to reduce alcohol-related harm in older people and help them to live healthier, more active and independent lives.”
Simon Antrobus, Chief Executive of Addaction, said: “Problem drinking doesn’t happen in isolation – there are always other factors involved. This is especially true for the over 50s who can end up drinking at harmful levels as they face challenging life transitions such as retirement, the loss of a loved one or loneliness.
“We’ve called our initiative ‘Drink Wise, Age Well‘. It’s a great opportunity for us to raise awareness of these issues and improve access to information and treatment for the over 50s. Addaction is delighted to deliver this comprehensive programme, supported by the considerable commitment and expertise of our consortium partners.”
Baroness Sally Greengross, Chief Executive of the International Longevity Centre UK, said: “There is no doubt that baby boomers are ‘behaving badly’, challenging preconceptions of what it means to be old and engaging in risky behaviours in terms of ‘drink, drugs and sex’.
“While drinking isn’t a problem per se, as a think tank that specialises in healthy ageing, we know that too much alcohol affects older people disproportionately and may have serious consequences for their physical and mental health and general wellbeing. Things can become particularly problematic, for example, when older people are on complex medication regimes and then drink too much. At best this may make their drugs temporarily ineffective and at worst it can lead to emergency hospital admissions.”
Controversy over new drug to treat alcohol dependence
A drug that can help people who are dependent on alcohol to cut down on the amount they drink, has been recommended in final draft Guidance by the National Institute for Health and Care Excellence (NICE).
The drug Nalmefene was granted a European Marketing Authorisation in February 2013, although that decision was criticised by some clinicians on the grounds that there were insufficient data to support the treatment.
The move to licence the drug in the UK has also proved controversial, dividing opinion among addiction experts, with some hailing the drug as a useful weapon in the armoury against alcohol problems while others attacked the move as an attempt to medicate away what is, in reality, a societal problem.
Nalmefene
In its draft guidance, NICE says Nalmefene should be available as an option for the mildly alcohol dependent, a criterion which excludes those with physical withdrawal symptoms, or who require immediate detoxification. The drug is intended to assist those who have sought help to reduce their drinking, and the marketing authorisation states that Nalmefene should only be prescribed in conjunction with continuous psychosocial support focussed on treatment adherence and reducing alcohol consumption. A course should only be started in patients who continue to have a high drinking risk level two weeks after initial assessment. A high drinking risk level is defined as at or above 60g per day of pure alcohol for men and 40g per day for women. This translates into an average daily consumption of 7.5 units of alcohol for men and 5 units for women. On the basis of these criteria, nearly 600,000 people will be eligible to receive the treatment.
Nalmefene (also called Selincro and manufactured by Lundbeck) is an opioid receptor modulator taken as a tablet once a day on an as-needed basis, which reduces the urge to drink. It is priced at £84.84 for a pack of 28 tablets. The drug is licensed for use alongside psychosocial support to help people reduce their alcohol consumption and give them the encouragement they need to continue with their treatment.
 Professor Carole Longson, NICE Health Technology Evaluation Centre Director, said:
Professor Carole Longson, NICE Health Technology Evaluation Centre Director, said:
“Alcohol dependence is a serious issue for many people. Those who could
be prescribed Nalmefene have already taken the first big steps by
visiting their doctor, engaging with support services and taking part in
therapy programmes. We are pleased to be able to recommend the use of
Nalmefene to support people further in their efforts to fight alcohol
dependence. When used alongside psychosocial support, Nalmefene is
clinically and cost effective for the NHS compared with psychosocial
support alone.”
Alcohol Concern Chief Executive, Jackie Ballard, said: “It is important that there are a variety of treatments available to support people who want help with their alcohol dependency.
“The introduction of Nalmefene will be a useful addition to the clinician’s toolbox, when used in conjunction with other treatment methods to tackle the harmful consequences of alcohol misuse.”
Professor Jonathan Chick, a consultant psychiatrist and Honorary Professor at Queen Margaret University Hospital, Edinburgh, and a Consultant to Lundbeck, said: “The decision by NICE to recommend Nalmefene for appropriate patients is important. Although for many people dependent on alcohol, abstinence is the preferred and optimal goal, Nalmefene represents an alternative step, helping people to cut down drinking to less harmful levels when they are not ready and have no medical need to give up alcohol altogether. This may help us to engage many alcohol dependent patients that we know are not currently receiving help.”
The critics
Professor Mark Bellis, Alcohol Lead for the Faculty of Public Health, said there were relatively simple alternatives that would reduce alcohol consumption without the need “to medicate the middle classes”, such as reducing advertising of alcohol and introducing a minimum price per unit.
He said: “Once again this is going to increase pressure on the NHS when there are alternatives that would reduce pressure on health services by cutting alcohol consumption.
“There are plenty of ways that don’t require prescribing – and the additional pressures on the NHS – which could reduce harmful drinking.
“We need to think very carefully about how we use limited resources and prescribe for people who, with relatively simple population interventions, such as reducing advertising and minimum unit pricing, could quite easily reduce alcohol consumption to safer levels.”
He added that Nalmefene reduced alcohol consumption by a relatively modest amount when compared with counselling alone and added that medicating people always came with the risks of side effects. He also said that it was not known whether the reduction in drinking was maintained in the long-term.
Dr Niamh Fitzgerald, a lecturer in Alcohol Studies at the Institute for Social Marketing (ISM) at the School of Health Sciences, University of Stirling, shared the misgivings:
“The fact that alcohol problems are widespread in society is an important principle for effective policy options such as minimum unit pricing and restrictions on marketing of alcohol.
“It would be unfortunate if the availability of Nalmefene led to a sense that the appropriate response to these widespread problems was for the NHS to medicate large numbers of people rather than initiating these other more effective and less costly approaches to reduce consumption.”
About-turn on closing times
Coalition Government rows back on abolition of “artificially early” closing times in the 2003 Licensing Act.
The latest Ministerial Guidance to the Licensing Act 2003, the government’s guidance to licensing authorities on how they should interpret the law, represents a partial abandonment of one of the fundamental assumptions of the Act as it was introduced by the then Labour Government.
This was that ‘artificially early’, fixed closing times were the main cause of heavy drinking and associated public disorder around closing times. The solution, therefore, was to abolish the system of permitted hours, allowing individual premises to trade as late into the night as they wished, unless there was some valid objection to their doing so, and the objection had to relate specifically to the individual premises: a blanket restriction on trading hours over a whole area was not permitted.
However the new Ministerial Guidance advises local authorities that “As part of its licensing policy, the licensing authority may also wish to consider the use of alternative measures such as fixed closing times, staggered closing times and zoning within its area, providing such mechanisms are justified on the basis of the licensing objectives and are only presumptive, with final decisions continuing to be made in relation to individual premises on a case by case basis in accordance with what is appropriate to promote the licensing objectives.”
This contrasts with the advice issued in 2004, which said: “Licensing areas should not set predetermined closing times for particular areas.”
The 2004 Guidance reflected the claims made by the Labour Government and its allies in the drinks industry and the media. The White Paper ‘Time for Reform’, which announced the changes, insisted that one of the main problems with the then current licensing arrangements was their actually causing public disorder “through standard closing hours which mean that large numbers of drinkers come out onto the streets late at night at the same time.”
The Labour Government also claimed that “artificial” closing times were an important cause of binge drinking as people tried to ‘beat the clock’.
No evidence in relation to the speed or volume of consumption in the period before closing time, compared with other periods, was provided. However, Labour MP, Jane Griffiths, then chairwoman of the All Party Parliamentary Group for Beer, wrote:
“The effect of (the) compulsory closure has been for people to drink ‘against the clock’, with whole generations of young people learning to drink as much as possible in a short space of time… Most of these young people are drunker than they would be if they drank at their own pace.”
The White Paper stated that “research indicates” that de-regulated closing times, by spreading the period during which customers leave, should produce the following key outcomes:
- A more gradual and orderly pattern of dispersal of peak densities between the hours of 11pm -12 midnight, and 2am and 3am in urban centre
- Significant reductions in reports of drink-related offences and in arrests for such offences
- Reductions in binge drinking and drunkenness on the streets
These claims were contested, at the time, by the Institute of Alcohol Studies, amongst others, pointing out that the research to which the Government referred had been produced at the behest of the drinks industry. Critics also referred to international evidence suggesting that it was actually later closing times that were more closely associated with heavy consumption and the associated public disorder problems. In the event, evaluation of the impact of the Licensing Act 2003 suggested that the principal effect of the Act was to delay the peak time for crime and disorder until later into the night.
Commenting on the latest Ministerial Guidance, a Home Office spokeswoman said the Government’s position had changed after a 2010 consultation that showed support for zoning and staggered closing times.
Public support for Leicester street drinking ban
Hundreds of people across Leicester have backed plans for a city-wide ban on antisocial public drinking.
 A series of public consultations took place across the summer asking whether people supported plans for the police to have stronger powers to tackle problem street drinking linked to antisocial behaviour.
A series of public consultations took place across the summer asking whether people supported plans for the police to have stronger powers to tackle problem street drinking linked to antisocial behaviour.
Government legislation, known as Public Spaces Protection Orders, or PSPOs, gives police and police community support officers the power to tackle a wide range of antisocial behaviour problems linked to noise, alcohol and nuisance dogs.
Some controls on street drinking already exist in parts of the city centre, but the latest proposals would see those powers extended to cover the entire city under a PSPO.
In all, 630 people from the across the city took part in the public consultations. Of those, 87 per cent said street drinking was a problem in the city, and 77 per cent of people backed plans to bring in a city-wide ban.
Leicester City Council will now take the results of the consultation to the next meeting of the full council, on November 13, for a decision to be made.
Along with residents’ views, the consultations in Leicester also took into account information from city wardens, parks services, play services, cleansing teams and police neighbourhood officers.
About 73 per cent of people reported noise linked to street drinking as a problem, 70 per cent complained about littering, while 53 per cent said verbal abuse linked to street drinking was an issue.
Other problems linked to antisocial street drinking included intimidation, urination and vomiting, racism, begging and smashing glass.
Assistant City Mayor for Neighbourhood Services, Councillor Sarah Russell, said: “A very high number of people who took part in these consultations – 87 per cent – felt that street drinking and associated antisocial behaviour were real problems for them, and 77 per cent of people supported the idea of city-wide powers to tackle the issue.
“People have told us that they’re suffering with the noise, littering, intimidation, verbal abuse and other unpleasant behaviour linked to street drinking, and this PSPO will give the police greater powers to take action.”
The PSPO would cover anywhere within the city boundary, meaning it can be used to tackle drinking-related antisocial behaviour anywhere where problems are reported.
Officers can order people drinking in these areas to stop, hand over any alcohol or dispose of the alcohol, with people who fail to do so facing a spot fine of up to £100, or up to £1,000 if the case goes to court.
92% of people feel ashamed to drink and drive as 50th anniversary THINK! campaign is launched
The Department for Transport has lauded the success of the anti-drink drive publicity campaign which, in 2014, celebrates its 50th anniversary.
New research from THINK!, the Department’s road safety education arm, shows how much attitudes have changed to drink-driving in the last half century.
However, the Department’s focus on the publicity campaign is likely to be criticised as playing down other factors, most noticeably the 1967 Road Safety Act, which established the 80mg% legal alcohol limit for drivers and introduced the breathalyser.
The Publicity Campaign
The THINK! survey found that of those surveyed, 91 per cent agreed that drink-driving was unacceptable and 92 per cent of people said they would feel ashamed if they were caught drinking and driving. This compares to over half of male drivers and nearly two-thirds of young male drivers who admitted drink-driving on a weekly basis in 1979.
The Department says that the shift in attitudes is a stark contrast to the first drink-drive public information film in 1964, which was set in an office Christmas party. The advert politely reminded people that “four single whiskeys and the risk of accident can be twice as great… If he’s been drinking, don’t let him drive.”
Through a combination of road safety campaigning and better enforcement, road deaths due to drink-driving have fallen from 1,640 in 1967 to 230 deaths in 2012. Recently, the Government is sending out a clear message that there is still a long way to go. The new advert reminds people that one death on our roads is too many.
Transport Secretary, Patrick McLoughlin, said:
“The change in attitudes to drink-driving over the last 50 years is a huge success story. It is hard to imagine now how shocking and ground-breaking the first drink-drive campaigns were when they launched. Clearly THINK! has had a significant impact.
“Most of us understand drink-driving wrecks lives but there is further to go. In 2012, 230 people were killed in drink-driving accidents – 230 too many. This makes the THINK! campaign as relevant as ever.”
Recently, over 88 per cent of people say that they would think badly of someone who drinks and drives and almost half of respondents say they would prefer to tell their partner they watch pornography regularly than confess to being caught drink-driving (45 per cent). The survey also showed that 61 per cent of people would rather reveal their internet search history to their employer than admit to a drink-drive conviction, with 24 per cent who would rather tell their partner they’ve had a sexually transmitted infection (STI).
Shaun Helman, Head of Transport Psychology at the Transport Research Laboratory says:
“Compared with 50 years ago, drink-driving is now very much minority behaviour. This change has been achieved through firm laws, highly visible enforcement, and a sea-change in public attitudes; drink-driving is now frowned upon by the vast majority of people.”
However well executed the anti-drink drive advertising campaign had been, it is unlikely it would have achieved the reduction in casualties that has been achieved in the absence of changes to the law and the way it is enforced. The chief legal change was the introduction of a per se law making it illegal to drive a motor vehicle with a blood alcohol level exceeding a defined amount (80 milligrammes of alcohol per 100 millilitres of blood), the equipping of police with breathalysers to conduct roadside tests for alcohol, and, by international standards, relatively severe penalties on conviction.
The per se law was introduced by Minister Barbara Castle in the 1967 Road Safety Act. It took years to come into being. It was introduced in the face of strong opposition but it has since been acknowledged as one of the most successful pieces of road safety legislation ever passed. The legal alcohol limit for drivers that was set in 1967 remains in force in the UK, although Scotland has announced it will reduce the limit.
Milestones to Breath Testing:
1872 – Licensing Act made it an offence to be “drunk while in charge on any highway or other public place of any carriage, horse, cattle or steam engine”.
1925 – The 1872 offence was extended to cover “any mechanically propelled vehicle”.
1927 – The BMA published “Tests for Drunkenness” responding to concerns of motorists charged with serious offences being given the chance of a fair defence. In the same year the Court of Appeal quashed the conviction of a person a jury had found guilty of being incapable of driving a car through alcohol though he was not “drunk” in the conventional sense! The learned judge remarked that “drunk” is what an ordinary reasonable person would consider as such.
1932 – Professor Widmark of the University of Lund, Sweden, provides the means for scientific testing of the amount of alcohol content in the blood. Such testing was adopted in Scandinavian countries.
1932 – “If you drink don’t drive. If you drive don’t drink.” Poster message first issued by the United Kingdom Alliance.
1935 – BMA publish “Relation of Alcohol to Road Accidents” at request of the Minister of Transport, Mr Hore Beliksha.
1936 – United Kingdom Alliance begins campaign for introduction of scientific testing for blood alcohol concentration in UK.
1939 – House of Lords Select Committee recommend testing to be carried out on a voluntary basis with the hope that at a later date the public will be so educated as to agree that these tests should be made obligatory.
1951 – “Don’t drink and drive” message taken up by Ministry of Transport in Christmas broadcast.
1954 – BMA report on “Recognition of Intoxication”.
1959 – Medical Research Council publish the report “Effects of small doses of alcohol on a skill resembling driving “ by Professor G C Drew.
1960 – BMA report “Relation of alcohol to road accidents”.
1962 – Borkenstein’s Grand Rapids study.
1962 – Road Traffic Act allowed a police constable to request a sample of blood or urine from an accused motorist but did not make it compulsory nor did it set an alcohol limit.
1963 – 132 deaths on the roads over Christmas with Road Research Laboratory stating “consumption of alcohol was the main factor in increasing the casualty rate”.
1965 – Publication of White Paper “Road Safety Legislation 1965-66” by Tom Fraser, Minister of Transport
1966 – Barbara Castle introduces Bill. Delayed by General Election but re-introduced after the Labour Government’s re-election.
Scotland: Lower drink-drive limit before Christmas
Justice Sec aims to lower blood alcohol limit from 80 to 50mg per 100ml for early December.
 Justice Secretary Kenny MacAskill has introduced an order in Parliament which will mean that, subject to approval, a reduced drink-drive limit will come into effect on December 5 2014, in time for Christmas and the New Year.
Justice Secretary Kenny MacAskill has introduced an order in Parliament which will mean that, subject to approval, a reduced drink-drive limit will come into effect on December 5 2014, in time for Christmas and the New Year.
Under the plans, the blood alcohol limit in Scotland will be reduced from 80mg in every 100ml of blood, to 50mg in every 100ml of blood, bringing Scotland into line with most other European countries.
The Scottish Government previously announced the intention to reduce the limit, following a consultation which found almost three-quarters of those who responded believed the drink-drive limit should be reduced.
The consultation responses suggested the likely benefits of a lower limit would be fewer road accidents and fewer casualties, with Scotland’s roads currently seeing 20 deaths a year involving drivers who had been drinking and driving.
A multimedia marketing campaign to raise awareness of the new lower limit will be launched in the coming weeks.
Kenny MacAskill said: “The latest estimates show that approximately one in ten deaths on Scottish roads involve drivers who are over the legal limit and research shows that even just one alcoholic drink before driving can make you three times as likely to be involved in a fatal car crash. As a result, 20 families every year have to cope with the loss of a loved one and around 760 people are treated for injuries caused by someone who thought it was acceptable to drink alcohol and get behind the wheel and drive. We cannot let this continue.
“This new limit will bring Scotland into line with most of Europe and send a clear message to drivers who continue to ignore the warnings that there is never an excuse to drink and drive.
“Lowering the drink drive limit will help make Scotland’s roads safer, it is the right thing to do, and most importantly, it will save lives meaning that fewer families have to go through the heartache of a loved one lost.”
Sandy Allan, RoSPA (Scotland) Road Safety Manager said:
“RoSPA welcomes and strongly supports the Scottish Government’s decision to lower the drink-drive limit in Scotland, which we believe will save lives and prevent injuries on Scotland’s roads. There is a considerable body of research which shows that reducing drink-drive limits is effective in reducing drink-drive deaths and injuries. We would like to see the rest of the UK follow Scotland’s example.”
New SHAAP report focusses on alcohol and brain damage in teenagers
Scottish Health Action on Alcohol Problems has published a review of the evidence on Alcohol and the Developing Adolescent Brain.
 The review points to emerging evidence that the adolescent brain may be especially vulnerable to alcohol harms. Brain development continues until the mid-twenties, and there is clear evidence that suggests a likely causal association between alcohol use in adolescence and structural changes to the brain.
The review points to emerging evidence that the adolescent brain may be especially vulnerable to alcohol harms. Brain development continues until the mid-twenties, and there is clear evidence that suggests a likely causal association between alcohol use in adolescence and structural changes to the brain.
The review argues that this evidence should inform all health promoting activities and should prompt investment in further exploratory research.
It also argues that protecting young people from alcohol-related harm should be embedded in national and local policy and should be within the context of a ‘whole population’ approach to reduce overall alcohol consumption.
Commenting on the report, SHAAP Chair Dr Peter Rice said:
“This report is a summary of the current state of knowledge on alcohol and the developing brain. This is a rapidly evolving area of research and this report is a staging post rather than the last word. However, it is clear that there a several grounds to be concerned about the effects of alcohol on the brain, which is in development into the mid-20s.
“The uncertainties and known risks need to be better understood by professionals and the public. The emerging evidence supports a cautious approach to the use of alcohol by young people and for parents, “the later the better” is the best advice.”
Children’s Commissioner says more must be done to protect children from parents’ problem drinking
Inadequate attention is still being paid to the children of problem drinking parents, according to a new report from the Children’s Commissioner.
 The report argues that some local services for adults with alcohol problems and staff in children’s services may fail to identify children’s needs adequately and assist them in getting help or protection. It also finds that local services do not all work together effectively to measure and address the impact on children of parental alcohol misuse.
The report argues that some local services for adults with alcohol problems and staff in children’s services may fail to identify children’s needs adequately and assist them in getting help or protection. It also finds that local services do not all work together effectively to measure and address the impact on children of parental alcohol misuse.
Commissioned by the Office of the Children’s Commissioner from The Children’s Society, the report “I think you need someone to show you what help there is,”: Parental alcohol misuse – uncovering and responding to children’s needs at a local level looks at ways of estimating the number of children affected by parental alcohol misuse and at the help available to them. Based on research with children and young people, alcohol misusing parents and professionals who work with them in three areas of England, the study identifies the steps service providers and co-ordinating bodies – including health and social care services – need to take to address children’s safety and diminish the impact of problem drinking on children. These include the need to share information consistently across services and to develop joint approaches to commissioning and effective local strategies involving all agencies. Those working with adults should also receive training to help them talk to parents who misuse alcohol about the impact their drinking may be having on their children, and all those working with children and families need training to assist them in recognising the difficulties children may be experiencing so that they can get help.
The report follows the publication of Silent Voices by the Office of the Children’s Commissioner in 2012, which reported that nearly one in three (30 per cent) children live with at least one parent who is a binge drinker and a fifth (22 per cent) live with a hazardous drinker. It recommends Health and Wellbeing Boards and Local Children’s Safeguarding Boards work together closely to identify and support children in families where there is alcohol misuse.
Talking about the impact that parental alcohol misuse has on children, a 13 year-old girl who took part in the study said: “The anger goes round and round in my head, I get dizzy and hot and I can’t cope, I just burst. I have anger issues.”
A 16 year-old girl said, “I realised when I went into care that this didn’t have to be the way.”
Maggie Atkinson, Children’s Commissioner for England, said, ‘Children have a right to be kept safe from harm and adults have a duty to protect them, and this includes the damage caused by parents’ alcohol misuse. Parents and carers must be made aware of the effects their problem drinking can have on children and young people, and health and social care services must get better at providing effective co-ordinated responses. Problem drinking is frighteningly common. It not only causes problems for the drinker but also all those around them, including their children. The social and economic cost is immense.’
Joanna Manning, National Lead on Substance Misuse for The Children’s Society, said: ‘Children and young people are suffering the impact of their parents’ drinking for a long time before it comes to the notice of the authorities – if at all. Even then, the routes to help and the services available are ad hoc and vary across the country. Too many people are in denial about the scale of the problem and the level of harm caused. It’s also the case that local authorities tend to focus on young people’s own drinking without consideration that it might be learnt or normalised behaviour from their parents. Equally, not enough is being done to address and support parents who drink, in order to reduce the impact upon children and families’.
Wales: Stark challenges posed by alcohol
The stark challenges posed by alcohol are outlined in a new publication, Alcohol and health in Wales 2014, published by the Public Health Wales Observatory.
 The report discloses that every week in Wales alcohol causes 29 deaths – around 1 in 20 of all deaths. Most result from long-term drinking and its role in increasing the risk of some cancers, cardio-vascular disease and other illnesses.
The report discloses that every week in Wales alcohol causes 29 deaths – around 1 in 20 of all deaths. Most result from long-term drinking and its role in increasing the risk of some cancers, cardio-vascular disease and other illnesses.
The impact of alcohol on health also creates enormous pressure on the health system. Every week, Welsh hospitals handle as many as 1,000 alcohol-related admissions.
Drinking in children and young people remains a particular concern, with 17 per cent of males and 14 per cent of females aged 11–16 drinking alcohol at least once a week – higher than in England and Scotland and twice that of the Republic of Ireland.
While the report shows that all parts of Wales are touched by alcohol, the most deprived communities suffer substantially higher levels of both alcohol-related diseases and deaths.
The report does show a decrease in heavy drinking among adults aged under 45, particularly in males and the youngest females; however, heavy drinking has increased or stayed the same for adults aged 45+.
Professor Mark Bellis, Director of Policy, Research and Development at Public Health Wales, said: “While we are making progress, this new report shows much more is still to be done if we are to reduce the avoidable harms that alcohol causes to communities across Wales.
“We need to help people make the right choices about their own drinking. Too many drinkers fail to recognise how even moderate drinking can increase their risks of developing diseases such as cancer. The normalisation of drinking at a young age is also especially harmful and our problems with alcohol must be tackled early in life.”
Andrea Gartner, project lead for the report, added: “This new report provides a comprehensive analysis of alcohol consumption patterns and the impact of alcohol on health. It will provide stakeholders with the necessary information to inform action and drive change.”
Substance misuse in Wales 2013-14
Welsh Government data has also revealed the extent to which alcohol affects patients under treatment for substance misuse.
The latest Annual Profile of Substance Misuse in Wales report (2013-14) found that of the 24,806 referrals in 2013-14 (excluding DNAs before assessment), alcohol was the main problematic substance reported in the majority (54.2%) of cases (13,447). Alcohol was cited as the only substance in 12,072 cases (48.7% of total referrals). The number of alcohol misuse cases increased on 2012-13 (13,285) while the number of drug cases declined.
However, the standout figure from the datasets concerns older people (50+ year-olds). The report states that “the older age group is the only age group in which referrals to substance misuse treatment services is increasing. Overall, referrals for any alcohol or drug misuse in this age group have increased by 15.8 per cent over the five-year period 2009-10 to 2013-14.” In particular, the biggest increase in referrals in the last 12 months was among 60+ year-olds.
Other headline data from the report:
- In 2014 there were three times more hospital admissions for alcohol specific conditions compared to illicit drug poisonings (11,869 admissions and 3,962 admissions respectively). This trend has remained relatively consistent year on year over the last 6 years.
- In the last year, alcohol related deaths numbers were 3.4 times higher than drug misuse deaths (467 and 135 deaths respectively).
- Whilst the number of hospital admissions for alcohol specific condition (any position) is gradually decreasing, with a total of 15,071 admissions in 2012, admissions for broad measure alcohol-attributable conditions are increasing over time with 34,077 admissions in the same year.
- Self-report ‘drinking above guidelines’ has decreased from 51.3 per cent to 48 per cent amongst males and from 37.8 per cent to 36 per cent in females over the six year period. The self-report data on ‘binge drinking’ followed a similar trend in females with a decrease from 21.8 per cent to 20.5 per cent, however, amongst males the proportion decreased from 34.3 per cent in 2008 to 30.8 per cent in 2012 but in the last year rose to 31.9 per cent.
- In 2013-14, there were a total of 3,099 admission for primary alcohol specific diagnosis and 11,869 admissions for alcohol specific diagnosis in any position.
Alcohol, drugs and tobacco joint strategic needs assessment support pack
Public Health England’s alcohol, drugs and tobacco division has published a Joint Strategic Needs Assessment (JSNA) support pack to help local areas develop joint strategic needs assessments and local joint health and wellbeing strategies that effectively address public health issues relating to alcohol, drug and tobacco use.
 The support pack, which is now in its third year, and is reviewed and updated annually, consists of eight resources covering young people’s substance misuse and adult alcohol, drug and, for the first time in 2014, tobacco use.
The support pack, which is now in its third year, and is reviewed and updated annually, consists of eight resources covering young people’s substance misuse and adult alcohol, drug and, for the first time in 2014, tobacco use.
For each topic area there are good practice evidence-based prompts to support local areas to assess need, and plan and commission effective services and interventions. The second component for each topic is a bespoke data pack for every local authority to support needs assessment and commissioning.
Joint Review – Public Health England and the Association of Directors of Public Health
This joint review of drug & alcohol commissioning by local authorities in England was published on 3rd October 2014 along with a covering letter from PHE Chief Executive Duncan Selbie, and ADPH President Dr Janet Atherton.
This followed a snapshot review of commissioning across local authorities in England to identify where there have been changes to commissioning and its impact on outcomes, as well as future plans for commissioning.
In welcoming the publication of the report, Dr Janet Atherton commended this collaborative approach, which will serve as a strong basis for continuing sector-led improvement of substance misuse services and result in improved outcomes for local populations.
Podcast
Our monthly podcast features interviews with experts from across the sector.
Gambling industry harms and parallels with the alcohol world
Will Prochaska –
Coalition to End Gambling Ads