In this month’s alert
Coalition pioneers minimum unit alcohol pricing
The Prime Minister is leading Government action on tackling drink-fuelled violence and the binge-drinking culture that fuels it. A new Alcohol Strategy sets out a radical approach to turn the tide against irresponsible drinking which costs the UK £21billion a year.
It will help reverse a culture that led to almost one million alcohol-related violent crimes and 1.2 million alcohol-related hospital admissions last year alone. Strategy highlights include:
- a minimum unit price for alcohol
- banning the sale of multi-buy discount deals
- zero tolerance of drunken behaviour in A & E departments
- a late night levy to get pubs and clubs helping to pay for policing and improved powers to stop serving alcohol to drunks
The Prime Minister said:
“Binge drinking isn’t some fringe issue, it accounts for half of all alcohol consumed in this country. The crime and violence it causes drains resources in our hospitals, generates mayhem on our streets and spreads fear in our communities.
“My message is simple. We can’t go on like this. We have to tackle the scourge of violence caused by binge drinking. And we have to do it now.
“So we’re going to attack it from every angle. More powers for pubs to stop serving alcohol to people who are already drunk. More powers for hospitals not just to tackle the drunks turning up in A&E – but also the problem clubs that send them there night after night. And a real effort to get to grips with the root cause of the problem. And that means coming down hard on cheap alcohol.
“When beer is cheaper than water, it’s just too easy for people to get drunk on cheap alcohol at home before they even set foot in the pub. So we are going to introduce a new minimum unit price – so for the first time it will be illegal for shops to sell alcohol for less than this set price per unit. We’re consulting on the actual price, but if it is 40p that could mean 50,000 fewer crimes each year and 900 fewer alcohol related deaths per year by the end of the decade.
“This isn’t about stopping responsible drinking, adding burdens on business or some new kind of stealth tax – it’s about fast immediate action where universal change is needed.
“And let’s be clear. This will not hurt pubs. A pint is two units. If the minimum price is 40p a unit, it won’t affect the price of a pint. In fact, pubs may benefit by making the cheap alternatives in supermarkets more expensive.
“Of course, I know this won’t be universally popular. But the responsibility of being in government isn’t always about doing the popular thing. It’s about doing the right thing.
“Binge drinking is a serious problem. And I make no excuses for clamping down on it.”
The Government Alcohol Strategy: Choice, Challenge and Responsibility sets out a plan to reduce binge-drinking in a bid to drive down crime and tackle health issues that for too long have gone hand-in-hand with drinking to excess.
This is NOT about stopping sensible, responsible drinking or penalising pubs. A minimum unit price will not affect the price of a pint in the local. In fact, pubs may benefit from making cheap alternatives in supermarkets more expensive.
A minimum unit price for alcohol will be introduced, meaning that, for the first time, alcohol will not be allowed to be sold below a fixed price per unit. This will put an end to cheap white ciders, spirits and super-strength lagers.
The Government will consult on the level of the minimum unit price, but expects it to be around 40p per unit. This will end the scandal of beer that is cheaper than water, and will tackle ‘pre-loading’ – drinking cheap alcohol at home before heading to the pub or nightclub. We will consult on this over the summer with a view to introducing legislation as soon as possible.
We will also consult on stopping multi-buy promotions like buy one, get one free promotions where consumers are encouraged to buy more than they want, while keeping good value for customers like half-price deals.
The strategy is designed to take fast action where immediate and universal change is needed and is not a stealth tax, a regulatory burden on businesses, or a bid to end responsible drinking.
Chief Constable Jon Stoddart, Association of Chief Police Officers lead on alcohol, said:
“Week in week out in town centres across the country the police have to deal with the consequences of cheap alcohol and irresponsible drinking.
“The growing trend for ‘pre-loading’ means that young people are often drunk before they even enter a bar. By the time they hit the streets at closing they are more likely to get involved in crime and disorder or injure themselves or others.
“I welcome the government’s new approach that will help reduce the availability of cheap alcohol, give communities a greater say over licensing in their area and reduce pressure on the police.”

Professor Sir Ian Gilmore, of the Royal College of Physicians and the Alcohol Health Alliance, said:
“Health care workers who struggle every day to cope with the impact of our nation’s unhealthy drinking will welcome tough new policies in areas such as price and licensing that are based on evidence and should bring about real benefits.”
Promoting lower strength drinks
The initiative, announced by Health Secretary Andrew Lansley, is designed to reduce sales of alcohol units and is being spearheaded by 34 leading companies behind brands like Echo Falls, First Cape and Heineken. It will result in a greater choice of lower strength alcohol products and smaller measures by 2015. Key commitments include new and lighter products, innovating through existing brands and removing products from sale. They include:
- Sainsbury’s have pledged to double the sales of lighter alcohol wine and reduce the average alcohol content of own brand wine and beer by 2020
- 25 milliion units will be gradually removed from Accolade Wines including Echo Falls Rose and Echo Falls White Zinfandel
- Brand Phoenix have committed to taking 50 million units of alcohol out of their wines by reducing 0.8% ABV on all FirstCape full strength red wines
- Molson Coors, the UK’s largest brewer, has committed to remove 50 million units by December 2015
- 100 million units will be removed by Heineken
- Own brand super-strength lager will be removed from sale by wholesaler Macro
- Tesco, the leading retailer for low alcohol drinks, will reduce the alcohol content of its own-label beer and cider and expand its range of lower alcohol wines and beers, already the biggest selling range in the UK
However, skepticism about NUP is not confined to sections of the alcohol industry. The independent think tank the Institute of Fiscal Studies also questioned the policy, arguing that a preferable approach would be to introduce a floor price for alcohol through the duty system, moving towards a more equal tax treatment of alcohol by type and strength combined with a restriction on selling alcohol below the total tax levied on it. Such a system could be designed to achieve an increase in the price of low cost alcohol similar to that from a minimum price. But it would have the advantage, the IFS says, of raising money for the Exchequer, whereas a minimum price would transfer revenues to the alcohol industry instead. If set at 40p, the IFS estimate that these transfers could be as much as £850 million per year.
Health Secretary Andrew Lansley said:
“Cutting alcohol by a billion units will help more people drink sensibly and within the guidelines. ….Estimates suggest that in a decade, removing one billion units from sales would result in almost 1,000 fewer alcoholrelated deaths per year, thousands of fewer hospital admissions and alcoholrelated crimes, as well as substantial savings to health services and crime costs each year.”
Mark Bellis, Faculty of Public Health and co-Chair of the Responsibility Deal Alcohol Network said:
“The past thirty years have seen a steady increase in the strength of beers and wines. Reversing this trend by switching sales to lower strength drinks could help reduce the alcohol problems we’ve seen grow over recent decades. Making this pledge work is not just about increasing sales of lower alcohol drinks. For real public health benefi ts, industry must also reduce sales of higher strength products.”
MP calls for more tax on super-strength cider
The former chairman of the All-Party Parliamentary Beer Group has called on the Government to crack down on super strength cider because producers are targeting the drinks at young people.
Alan Meale MP noted in the Early Day Motion (EDM) that super strength ciders cause health problems including speeding up the rate of liver cirrhosis.
He added that the drinks are taxed at “only half the amount charged on lager”, and take home high-alcohol ciders sell for as little as 16 pence per unit.
The MP for Mansfield also stated that cider sales in the UK have again risen with 47% of drinkers now regularly having a glass, compared to 42% less than a decade ago; and sales have increased from 1.7bn in 2006 to 2.4bn in 2011.
Fourteen MPs have signed the petition so far. Meale said: “This is something I raise around this time every year because I have always found the differences in tax between cider and beers. It is not about the regional producers, this is about the big companies producing a high range of high alcohol products. All the medical evidence shows that it can be very harmful.“
Beers and lagers are being heavily taxed whereas the super strength drinks that are being targeted at young people are available at half the price.”
NHS Alcohol Statistics – the war of numbers
The launch of the Coalition Government’s new alcohol harm reduction strategy coincides with another change to the way in which the statistics of alcohol-related admissions to NHS hospitals are collected and presented. On this occasion, the result is that the number of admissions appears to have declined rather dramatically.
The number of admissions is, of course, an issue of fundamental importance because these figures are one of the key indicators used to measure the size and significance of the national alcohol problem, and they are one of the determinants of the estimates made of the size of the economic burden placed by alcohol on NHS budgets and on the public purse. Clearly, the higher the number of alcohol-related admissions to hospitals there are, the greater the economic and social burden of alcohol appears to be. And, of course, the greater the problem is perceived to be, then the greater the pressure for policy measures to ameliorate it.
The Coalition’s New Improved Figures
The change in the Coalition Government’s approach to the numbers issue became apparent when, in advance of the launch of the new alcohol strategy, Prime Minister David Cameron made a highly publicised speech in which he promised to tackle the scandal of the binge drinking culture and the burden it places on society, and on the health service in particular.
Mr Cameron said:
“In 2010/11 alone there were 200,000 hospital admissions with a primary alcohol-related diagnosis, 40 per cent higher than in 2002/03. The number of patients admitted with acute intoxication has more than doubled to 18,500 since 2002/03.” Mr Cameron went on to say that the figures show an ever-growing bill to the NHS, which currently stands at £2.7bn a year, including £1bn on accident and emergency services. £2.7bn equates to £90 for every taxpayer. This is part of a wider cost to society from alcohol of between £17 billion and £22 billion per annum.”
Mr Cameron’s reference to the figures for 2010/2011 may have been a mistake, because the figures he quoted are more probably for 2009/2010. But the significant point is that the figure of 200,000 is a fraction of the figures that had previously received much media attention, the headline claim being that alcohol-related hospital admissions in England had passed the million mark.
What the figures mean
The difference between 200,000 and over a million is the difference between admissions where there was a primary diagnosis of a disease or a condition wholly attributable to alcohol, and the much larger number of admissions in which alcohol was recorded as a secondary or accompanying factor. (see graph below)
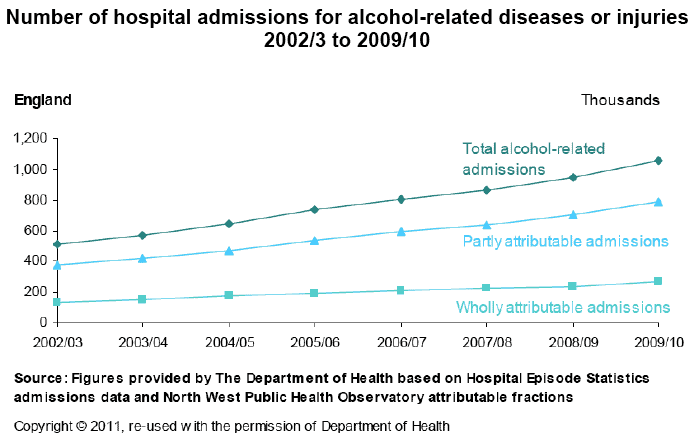
It appears that the Coalition Government is now minded to revise the way the alcohol admissions statistics are presented to show only those where alcohol entered into the primary diagnosis. Under the new Public Health Outcomes Framework, the North West Public Health Observatory will undertake a consultation on the methods used to measure alcohol-related admissions, and the definition adopted will be informed by the results of that consultation. However, the fact that Government Ministers are already referring to the lower figures suggests that the decision to change the system has already been taken.
What was wrong with the old figures?
Headlines about a million plus alcohol admissions to hospitals are indisputably very bad publicity for the alcohol industry, and it is understood that industry groups have been making representations to Government to change the way the figures are presented.
However, the old method of presentation had also been criticised by some more impartial commentators who argued that changes in the way alcohol admissions were recorded made comparisons with earlier years worthless and claims about a million plus admissions extremely questionable.
The key argument is that the method of coding hospital admissions has encouraged NHS hospitals artificially to inflate the number of admissions related to alcohol.
The issue is that the million plus figure is based on taking into account all the conditions recorded for each patient, not just the one for which the patient is actually admitted. Nigel Hawkes, the science journalist and founder of the Straight Statistics website, points out that many seriously-ill patients are admitted with several conditions: a lung cancer patient might, for example, additionally suffer from high blood pressure. The high blood pressure is not the condition for which the patient is being treated and it is not responsible for the admission to hospital, but it will also be recorded on his or her notes, and ‘coded’ by clerks. Lung cancer is not an alcohol-related disease, but high blood pressure is, with alcohol being implicated in around one third of cases. Hence, of every ten admissions to hospital of this kind, around three will be recorded as alcohol-related, even though alcohol was not the cause of the admission.
Hawkes writes:
“This might not matter much, beyond greatly exaggerating the numbers harmed by alcohol, if it were not for the variation in coding practice over time and between hospitals. The introduction of payment by results by the NHS in England and the publication by health analysts …. of death rates for individual hospitals have encouraged hospitals to increase the number of codes attached to each patient.”
This is because, if a hospital can show that a patient who died in its care suffered a whole range of conditions on admission, then that death will count for less in the calculation of its Hospital Standardised Mortality Ratio (HSMR) and its official performance rating will improve commensurately. Health analysts have worked out that the average number of codes per patient in the NHS in England rose from just under 3 in April 2005 to almost 4.5 by December 2010, an increase of 50 per cent. If the number of codes increases, then so will the number of ‘alcohol-attributable’ codes. So, Hawkes argues, a rise of 50 per cent in alcohol-attributable admissions over that period can be accounted for simply by ‘coding creep’.
However, while there is clearly substance to Hawkes’ claim that changes to the coding system have exaggerated the increase in alcohol admissions over time, there is an even clearer danger that counting only those in which alcohol forms part of the primary diagnosis will result in a large underestimate. There is a range of conditions which are not defined in terms of alcohol but which are partly attributable to it, and which, therefore, contribute to a patient’s admission to hospital. To exclude these would be to engage in the opposite kind of misrepresentation.
HMRC’s strategy for stopping alcohol duty fraud
– Better than before, but still not good enough…
Duty fraud costs Exchequer over £1billion each year, and rising
Her Majesty’s Revenue and Customs’ renewed strategy for dealing with alcohol duty fraud, now covering wine and beer as well as spirits, is a significant improvement on the previous strategy and the Department has achieved some of its early objectives. However, a report by the National Audit Office* has found that there has been no tangible success achieved in working with industry to disrupt the illegal diversion of duty-unpaid alcohol back into the UK market. There has also been a low level of criminal sanctions against fraudsters.
Problem created by EU
Alcohol duty fraud is carried out primarily by organized criminals who exploit weaknesses in the supply chains of alcohol producers, wholesalers and distributors to divert goods onto the UK market without paying the taxes that are due.
Opportunities for excise fraud emerged effectively with the creation of the European Union (EU) single market on 1 January 1993. Until that time, the Department and customs authorities in other Member States had established tight control of excise goods to ensure duties were paid on the goods produced. However, once the European single market was established, businesses were legally free to move goods around the EU, and alcohol could be held in warehouses on a duty suspended basis until they were dispatched. The duty due on goods dispatched for UK consumption becomes due once the goods are released from the warehouses, and goods destined for export could travel without any duty being paid. As excise duty rates on alcohol are far higher in the UK than on mainland Europe, perpetrators of fraud have exploited this new regime. The fraudsters move alcohol products to the EU with excise duties unpaid, store the goods in warehouses on the near continent, release the goods onto the EU market and then divert them back into the UK. Products are then sold on to retailers, wholesalers or other parties, without UK excise being paid.
The Department estimates that the amount lost, due to alcohol duty evasion, could be as much as £1.2 billion in 2009-10, a significant rise from £850 million in 2008-09.
According to the National Audit Office report, there has been no success in reducing the volume of alcohol legally moved to other EU countries with excise duties unpaid, but then diverted back into the UK for illegal sale. The Department has recorded increased revenue from agents participating in the new Registered Consignee scheme. However, its scheme requiring traders to provide financial guarantees for the duty on alcohol being moved has been less successful as the guarantees required by the Department are far lower than the value of the duty on goods being moved. HMRC has made minimal progress working with industry to secure alcohol supply chains.
In each of the four years to 2009-10, there were convictions in just six cases or fewer for suspected alcohol duties fraud. The Department considers civil sanctions more effective in some cases. During 2010-11, the quantity of alcohol seizures increased to almost 10 million litres – an increase of 61 per cent. Amyas Morse, head of the National Audit Office, said:
“HMRC has estimated that the evasion of alcohol duty could have cost the taxpayer over £1 billion in 2009-10 – and the level of fraud is on the rise. While the renewed strategy to deal with this is more comprehensive than what went before, and the Department has had some early notable successes, it needs to do better in a number of areas. This includes establishing reliable estimates of the tax gaps for beer and wine and achieving tangible success in tackling the illicit diversion of duty unpaid alcohol back into the UK market.”
*National Audit Office: HM Revenue and Customs’ Renewed Alcohol Strategy: A progress report 2012 is available for download at: http://www.nao.org. uk/publications/1012/ hmrc_alcohol_strategy_ progress.aspx
New £1 million fund to tackle binge drinking
A new £1 million fund to give local communities the tools they need to tackle binge and underage drinking has been announced by the Government’s Champion for Active Safer Communities,
Baroness Newlove. Baroness Newlove is a community campaigner based in the North West of England and was made a peer in July 2010. Since the death of her husband Garry at the hands of drunken teenagers in 2007, she has worked to make communities safer. In October 2010 she was appointed the Government Champion for Active Safer Communities and spent six months at the Home Office where she wrote her first report ‘Our vision for safe and active communities’.
The announcement of the new fund came on the day Baroness Newlove published her latest report ‘Building Safe, Active Communities: Strong foundations by local people’, which is a collection of inspiring, yet practical lessons from those who are changing their neighbourhoods for the better, providing good advice, and highlighting some of the barriers that have stifled their growth. In her interim report to Government published in July last year, Baroness Newlove identified tackling problem drinking as her most urgent priority and she will continue to focus sharply on this in the months ahead. This new fund will give ten successful communities – based on models of grassroots projects already delivering for their neighbourhoods – the resources to tackle the alcohol issue locally.
Newquay
One claimed success is Newquay Safe Partnership. This brings together local councils, police, health workers, the Local Safeguarding Children’s Board, businesses, tourist chiefs, town planners and local residents to share information and deliver action. In the past two years the partnership has taken steps to curb the use of fake IDs, has prosecuted proxy buyers and targeted campaigns aimed at young people urging them to be responsible and for parents not to supply alcohol to children. Since 2009, the Cornish resort has seen an average fall of almost 30 percentage points in recorded antisocial and ‘rowdy’ behaviour.
Baroness Newlove said:
“I am sick of the harm caused by those young people who put themselves and others at risk from illegal drinking. The crime and antisocial behaviour that comes in its wake is a terrible blight on this country. It destroys the quality of life of innocent people and in the process sucks up huge amounts of public funding to repair the damage done to people and places.
“We need a new drinking culture in this country. I want to see responsible drinking, so we can rid our streets of drunken violence and intimidation. We need direct, effective action on the ground to make a difference, and make ‘sociable drinking’ the acceptable norm. This will not be achieved overnight, I realise. But we need to take action now and I am very pleased that the Government will shortly publish a long-term strategy on alcohol.
The report can be found at: www.communities. gov.uk/publications/ communities/ buildingsafecommunities
Disappointing results of Alcohol Arrest Referral Schemes
A Home Office evaluation of Alcohol Arrest Referral (AAR) schemes has shown largely disappointing results. Pilot schemes were first introduced by the Home Office in 2007, under the Labour Government, as a means of tackling the link between alcohol and offending, in particular in the nighttime economy. This was supported by the Labour Government’s alcohol strategy ‘Safe. Sensible. Social’. AAR schemes aimed to test whether the benefits of brief interventions to reduce alcohol consumption in health settings could be extended to a criminal justice setting, with the additional goal of reducing alcohol-related offending. The schemes aimed to target those arrested for alcoholrelated offences and used brief interventions to emphasise the role that alcohol might have played in their offending, thus becoming a motivational lever to reduce drinking.
However, overall, the evaluations do not suggest that AAR schemes successfully reduced re-arrest. Average costs per intervention across the pilot schemes varied from £62 to £826, but most schemes did not break even as they did not reduce re-arrests overall. There was some evidence of reduced alcohol consumption among those who received the intervention, but for a number of reasons this finding should be treated with caution.
Profile of arrestees
One of the key benefits from the evaluations was finding out more about the population of people who are arrested in the night-time economy. This information is usually difficult to ascertain as flagging in custody for alcohol-related crimes is not consistently recorded. Indeed the comparison groups for both evaluations had to be constructed using proxy measures to approximate this.
The evaluations found that the profile of arrestees was different from practitioners’ initial thoughts; most notably, there was a higher proportion of dependent drinkers than anticipated. Furthermore, an important finding was that individuals were not necessarily prolific arrestees: over 50 per cent had just one arrest for the offence triggering the intervention, meaning no previous or subsequent arrests in the six months either side of the arrest. This was one of the factors making it difficult for the intervention to have a substantial impact on arrest rates. It also raises questions about whether an offender centred approach is the most effective way of tackling night-time economy-related crime and disorder if this is not a prolific group of offenders.
Effectiveness of Alcohol Arrest Referral schemes
The evaluation found that, overall, there was no strong evidence to suggest that delivering alcohol interventions following arrest could impact on criminal justice outcomes, namely reducing re-offending. The evaluation identified several possible reasons for the relative lack of success:
-
- Brief interventions delivered in a custody suite are not an effective way to reduce alcohol-related offending
-
- The re-arrest rates for alcohol-related offending are low, meaning that this is not a prolific group of offenders and therefore it would be harder to make any impact on the re-arrest rate
-
- Insufficient screening was undertaken to target the clients most likely to respond positively to a brief intervention
-
- The intervention did not sufficiently address the criminogenic needs of those arrested
Home Office reports on evaluation of alcohol arrest referral pilot schemes are available at the following links:
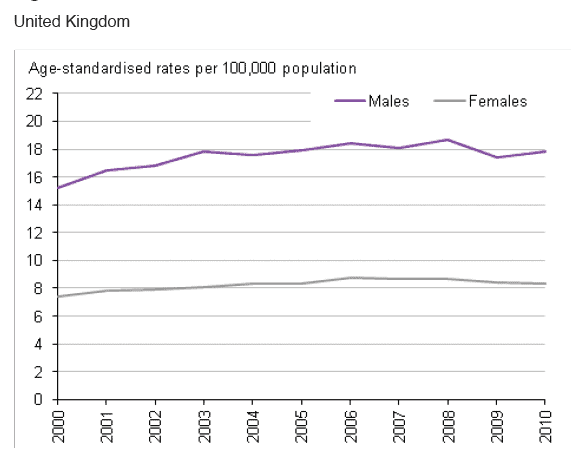
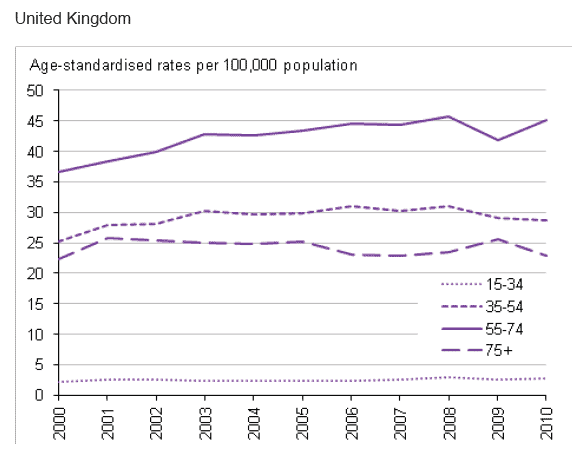
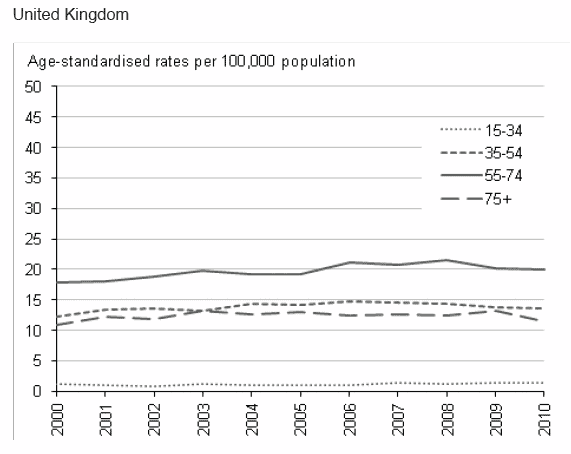
UK Alcohol-related deaths rise in 2010
In 2010 there were 8,790 alcohol-related deaths in the UK, 126 more than in 2009 (8,664). The increase was accounted for by males, female deaths falling slightly compared with the previous year. Since 2000, alcohol-related death rates have tended to increase in both sexes and in all regions. In England, death rates are highest in the North East and the North West. However, the rates in England as a whole are lower than in Wales, and they are still higher in Scotland.
The main findings from the Office of National Statistics are:
There are more alcohol-related deaths in males than in females, with 67 per cent of all alcohol-related deaths in the UK in 2010 being male
Alcohol-related death rates were highest for those aged 55-74 and lowest for those aged under 35 over the last ten years
UK males aged 55-74 years showed a sharp and statistically significant increase in alcohol-related death rate from 41.8 per 100,000 in 2009 to 45.2 per 100,000 in 2010
Alcohol-related death rates varied between the regions of England and tended to be highest in the North and lowest in the East of England over the last ten years
Within England and Wales, alcohol-related death rates are higher in Wales. In 2010 this difference was statistically significant.
Alcohol related death rates 2000-2010:
Alcohol related death rates by age group, males, 2000-2010:
Alcohol related death rates by age group, females, 2000-2010:
Source of graphs: Office for National Statistics, National Records of Scotland, Northern Ireland Statistics and Research Agency
New alcohol education campaigns launched in England and Scotland
New government alcohol health education campaigns have been launched in both England and Scotland. While separate, the two campaigns share the aim of warning drinkers of the dangers to health of regularly exceeding the sensible drinking guidelines.
Don’t let drink sneak up on you
The new Department of Health Change 4 Life campaign in England warns drinkers that there is an increased risk from serious illness, including heart disease, stroke and cancer, if they drink just a little bit more than they should. The campaign, including TV adverts, stresses that drinking even slightly over the lower-risk alcohol guidelines can seriously impact long-term health. The adverts highlight that regularly drinking around two large glasses of wine or two strong pints of beer a day triples the risk of developing mouth cancer and doubles the risk of developing high blood pressure.
A new survey for the Department of Health revealed that most people are unaware of the serious illnesses caused by drinking more than the guidelines.
For example:
- 85% of people did not realise it increases the risk of developing breast cancer
- 66% did not realise it increases the risk of bowel cancer
- 63% did not realise it increases the chance of pancreatitis
- 59% did not realise it increases the risk of mouth, throat and neck cancer
- 30% did not realise it increases the risk of high blood pressure; and
- 37% did not realise it reduces fertility
A new online calculator is available on the Change4Life website to help people check how much they are drinking and work out whether they need to cut down. Two million leaflets are also available for Change4Life supporters and health professionals around the country.
The campaign also offers handy hints and tips on how people can cut down – such as having booze free days, not drinking at home before people go out, swapping to low-alcohol or alcohol free drinks and simply using smaller glasses.
Secretary of State, Andrew Lansley said:
“It’s crucial we support people to know about how drinking too much poses risks to their health and how they can take control of their drinking. It can be easy to slip into the habit of having a few extra drinks each day, especially when drinking at home. But there can be serious health risks. Don’t let drinking sneak up on you.
“Change4Life is a fantastic, well known campaign, that has already helped a million families around the country. I want to expand it beyond eating well and moving more, so people look after themselves and really do live longer.”
Sarah Lyness, Executive Director of Policy and Information at Cancer Research UK, said:
“Alcohol can increase the risk of seven types of cancer, including two of the commonest kinds – breast and bowel cancers. And a recent study showed that nearly 12,500 cancers in the UK each year are caused by alcohol.
“The risk of cancer starts to go up even at quite low levels of drinking, but the more people cut back on alcohol, the more they can reduce the risk. Small changes can really make a difference – so try swapping a glass of wine or beer for a soft drink or having a few alcohol-free days a week.”
Scottish Campaign
The new Scottish Government’s Alcohol Behaviour Change campaign focuses on encouraging women to ‘Drop a Glass Size’ in 2012. Figures in the Scottish Health Survey show that around 38% of women regularly exceed daily and/or weekly sensible drinking guidelines. It is possible for a woman to exceed the weekly guidelines for less than £3. It is estimated that 1 in 30 female deaths in Scotland is alcohol-related.
The campaign encourages people to make small changes to the way they drink, such as alternating alcohol with soft drinks or water and having two alcohol-free days a week. The initiative, which also includes a national roadshow, aims to educate Scots about what they’re drinking, how much is too much and how they can moderate their drinking. As part of the campaign, a new ‘drinking time machine’ smart phone app has been developed to show people the shocking effects of regularly drinking too much. The app is available exclusively from the Scottish Government free for one month and will show users how alcohol speeds up the aging process. Cabinet Secretary for Health and Wellbeing Nicola Sturgeon said:
“Evidence shows us that most people who drink alcohol, particularly at home, have no idea of how much they are actually consuming. This campaign aims to show people how small changes to their drinking habits can have a significant impact on their health and wellbeing.
“Scotland’s unhealthy relationship with alcohol is now widely recognised and much has been done in the last five years to address this. Our alcohol framework outlined a package of over 40 measures to reduce alcohol-related harm. We have made considerable progress including banning quantity discounts and restricting promotions on off-sales. And we have invested a record £155 million over the last four years to tackle alcohol misuse.
“However I have been clear that there is more that can and must be done. Alongside educational efforts such as this campaign the introduction of the Minimum Pricing Bill is a significant step forward. There is a clear link between the price of alcohol and consumption levels, which is why we have always made the case for the introduction of a minimum price.
“The support in favour of minimum pricing is now overwhelming, and I hope that, this time around, Scotland’s MSPs will do the right thing and back this policy.”
Audrey Birt, Scotland Director at Breakthrough Breast Cancer, comments:
“We’re happy to be supporting this new campaign from the Scottish Government. We’ve known for some time that regularly drinking alcohol can increase the risk of developing breast cancer as well as causing other health problems. The good news is women can reduce their risk of developing the disease in a number of ways, including decreasing their alcohol intake, as well as maintaining a healthy weight and being physically active.”
The nationwide campaign will feature three different sized wine glasses to emphasise the central theme of the initiative. The three different sized wine glasses highlight that by making a small change such as dropping a glass size women can see and feel a big difference in their health and well-being now and in the long term.
New million pound fund to give local communities the tools to tackle binge and underage drinking
A new £1 million fund to give local communities the tools they need to tackle binge and underage drinking has been announced by the Government’s Champion for Active Safer Communities, Baroness Newlove. Baroness Newlove is a community campaigner based in the North West of England and was made a peer in July 2010. Since the death of her husband Garry at the hands of drunken teenagers in 2007, she has worked to make communities safer. In October 2010 she was appointed the Government Champion for Active Safer Communities and spent six months at the Home Office where she wrote her first report ‘Our vision for safe and active communities’.
The announcement of the new fund came on the day Baroness Newlove published her latest report ‘Building Safe, Active Communities: Strong foundations by local people’, which is a collection of inspiring, yet practical, lessons from those who are changing their neighbourhoods for the better, providing good advice, and highlighting some of the barriers that have stifled their growth. In her interim report to Government published in July last year, Baroness Newlove identified tackling problem drinking as her most urgent priority and she will continue to focus sharply on this in the months ahead. This new fund will give ten successful communities – based on models of grassroots projects already delivering for their neighbourhoods – the resources to tackle the alcohol issue locally.
Newquay
One claimed success is Newquay Safe Partnership. This brings together local councils, police, health workers, the Local Safeguarding Children’s Board, businesses, tourist chiefs, town planners and local residents to share information and deliver action. In the past two years the partnership has taken steps to curb the use of fake IDs, has prosecuted proxy buyers and targeted campaigns aimed at young people, urging them to be responsible and for parents not to supply alcohol to children. Since 2009, the Cornish resort has seen an average fall of almost 30 percentage points in recorded antisocial and ‘rowdy’ behaviour.
Baroness Newlove said:
“I am sick of the harm caused by those young people who put themselves and others at risk from illegal drinking. The crime and antisocial behaviour that comes in its wake is a terrible blight on this country. It destroys the quality of life of innocent people and in the process sucks up huge amounts of public funding to repair the damage done to people and places.
“We need a new drinking culture in this country. I want to see responsible drinking, so we can rid our streets of drunken violence and intimidation. We need direct, effective action on the ground to make a difference, and make ‘sociable drinking’ the acceptable norm. This will not be achieved overnight, I realise. But we need to take action now and I am very pleased that the Government will shortly publish a long-term strategy on alcohol.
The report can be found at: www.communities. gov.uk/publications/ communities/ buildingsafecommunities
More people dying from liver disease than ever before, with the disease being more common in the North and killing more men than women – Over one third of deaths alcohol-related
The number of people dying from liver disease in England is still rising, according to the first ever national report on the statistics published by the National End of Life Care Intelligence Network.
Deaths from liver disease: Implications for end of life care in England describes how there has been a 25% increase in liver disease deaths between 2001 (9,231 people) and 2009 (11,575 people). This is in contrast to other major causes of death, which have been declining.
Although numbers of deaths due to cancer, vascular or respiratory disease are still much greater, liver disease disproportionately kills people at a much younger age – a striking 90% of people who die from liver disease are under 70 years old. More than 1 in 10 of deaths of people in their 40s are from liver disease. When measured as ‘years of life lost’, liver disease is, therefore, much more prominent.
The report highlights that 60% of deaths from liver disease occurred amongst men and 40% amongst women. The single most common cause of liver deaths is alcohol-related liver disease, which accounts for well over a third (37%) of all liver disease deaths. However, the prevalence of deaths from alcohol-related liver disease varies greatly between males (41% of liver disease deaths) and females (30% of liver disease deaths). Alcohol-related liver disease is also more common in the most deprived areas (44% of liver disease deaths) than the least deprived areas (28% of liver disease deaths).
The complex needs of many patients who die from liver disease mean that more than two thirds die in hospital, compared to 55% of all deaths from any cause (2009).
Regional variation
Taking into account the diverse populations of each region, for example the South East having the largest population and London having a relatively younger population, the mortality rate due to liver disease varies between the regions. The age standardised mortality rate (2001-09) was highest in:
- North West (24.0 per 100,000, of which 11.4 were from alcohol-related liver disease)
- North East (21.9 per 100,000, of which 10.1 were from alcohol-related liver disease)
- London (20.2 per 100,000, of which 6.5 were from alcohol-related liver disease)
and lowest in:
- East of England (12.9 per 100,000, of which 4.9 were from alcohol-related liver disease)
- South West (14.3 per 100,000, of which 6.4 were from alcohol-related liver disease)
- South East (14.8 per 100,000, of which 5.8 were from alcohol-related liver disease)
Professor Martin Lombard, National Clinical Director for Liver Disease, urged people to consider the challenging and complex needs of those dying with this preventable disease. Professor Lombard said: “This report makes for stark reading about the needs of people dying with liver disease. Over 70% end up dying in hospital and this report is timely in helping us understand the challenges in managing end of life care for this group of people. The key drivers for increasing numbers of deaths from liver disease are all preventable, such as alcohol, obesity, hepatitis C and hepatitis B. We must focus our efforts and tackle this problem sooner rather than later.”
1 in 10 ambulance call outs down to alcohol in NE England
In a 1-year period, over 31,000 ambulance call outs were alcohol related in North East England, around 10 per cent of the total, and at a cost of millions to the public purse. These are the findings of a study carried out by a research team in Newcastle and published in the Journal Alcohol and Alcoholism*.
The researchers calculated that the cost of this ambulance work and the associated A&E attendances was over £9 million. If extrapolated to the whole country, the cost could be as much as £152 million per year.
It was found that, while alcohol related call-outs were most frequent in the 20–29 age group, around half of the alcohol related attendances occurred in individuals aged 30–59. The researchers suggest that this shows that alcohol related acute harm is not merely a feature of youth but is also relatively common in middle aged drinkers.
Unsurprisingly, street call outs were significantly more likely to happen on Fridays and Saturdays from 4 pm to midnight.
Violence
The data indicated that alcohol related ambulance call outs were three times more likely to involve verbal or physical abuse of staff compared with general ambulance work.
Other evidence shows that there are around 33 assaults per 1000 staff among ambulance staff nationally, compared with 14 per 1000 within Primary Care. Furthermore, A&E nurses are more than twice as likely as other frontline NHS staff (including doctors, ward nurses and receptionists) to experience verbal or physical abuse (78% compared with the UK average of 7%), with the main reason for the abuse given as the patient being under the influence of alcohol.
Underestimate
However striking their findings may be, the authors, nonetheless, caution that their findings may underestimate the full impact of alcohol related work in this area of emergency care. Firstly, paramedics are likely to focus on patients’ presenting symptoms and may not be able to assess less overt cases of alcohol related problems. These could include situations where they are dealing with victims of alcohol related physical or sexual violence, where the patient may not have been drinking. Also, patients with a flare-up of a chronic problem linked to drinking behaviour may not be detected. There is also the fact that many patients present themselves directly to A&E or are brought by family and friends rather than via ambulance.
*A Retrospective Analysis of the Nature, Extent and Cost of Alcohol-Related Emergency Calls to the Ambulance Service in an English Region : Martin, N; Newbury-Birch, D; Duckett, J; Mason, H; Shen, J; Shevills, C; Kaner, E; 2012. Alcohol and Alcoholism, 2012, 47(2): 191-197
Many young people don’t know what constitutes sensible alcohol consumption
Young people do not possess the knowledge or skills required to adhere to government guidelines for responsible alcohol consumption. This is the conclusion of a new British study published in the journal Drug and Alcohol Review.
Led by Richard de Visser, PhD, of the University of Sussex, researchers examined young people’s knowledge of, and use of, government guidelines for safe alcohol consumption.
A total of 309 secondary school students and 125 university students in England completed a survey regarding knowledge and beliefs. The university students also reported their alcohol consumption and completed tasks in which they poured their ‘usual’ drinks and what the government guidelines recommend for maximum ‘unit’ consumption on a daily and weekly basis.
Most respondents lacked the knowledge and skills required to drink in accordance with government guidelines.
Participants’ ‘usual’ drinks were substantially larger than one unit, and participants tended to underestimate the unit content of drinks.
For 5 of the 7 items examining knowledge and guidelines, fewer than half of the respondents gave correct responses.
Although university students gave a significantly greater number of accurate estimates than did school students, only a quarter of their estimates were within plus or minus 10% of actual content. The majority of estimates were underestimates: 52% among school students, 65% among university students.
“Our results mean that people’s reports of drinking patterns in research may lead to inaccurate estimates of the health effects of different levels of alcohol use,” de Visser notes. “There may be a need for more and/or different alcohol education in schools and the media.”
Heavy drinking on the decline
Contrary to the picture often presented of inexorable increases in alcohol consumption and harm, heavy drinking is, in fact, on the decline in Britain, according to the latest findings from the General Lifestyle Survey (GLS)*
The GLS is a continuous survey carried out by the Office for National Statistics to provide a picture of families and people living in private households in Britain, and covering a range of subject areas including drinking, smoking, education, employment and marriage, cohabitation and fertility.
On the 2010 GLS, respondents were asked two sets of questions about their drinking behaviour, resulting in measures of average weekly consumption and maximum amount drunk on any one day in the previous week.
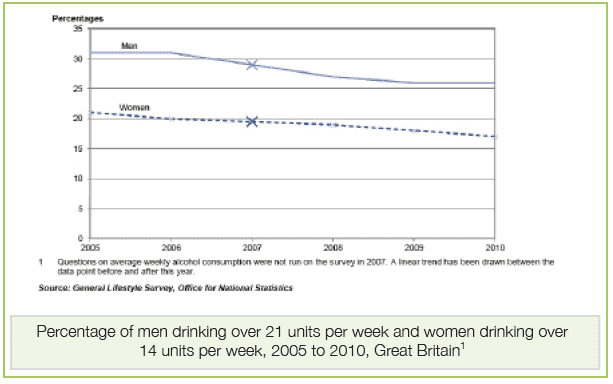
Trends in Alcohol Consumption: Main findings
Between 2005 and 2010, average weekly alcohol consumption decreased from 14.3 units to 11.5 units per adult. The decline was evident in both men and women.
Since 2005, there has been a decline in percentages of both men and women exceeding the old ‘sensible limits’ of 21 units per week for men and 14 units per week for women.
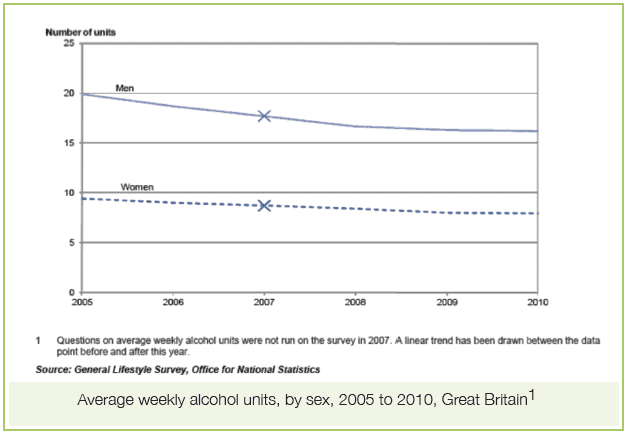
There have also been declines in the proportions of men and women classed as heavy drinkers, men drinking 50 or more units per week, women drinking 35 or more units per week.
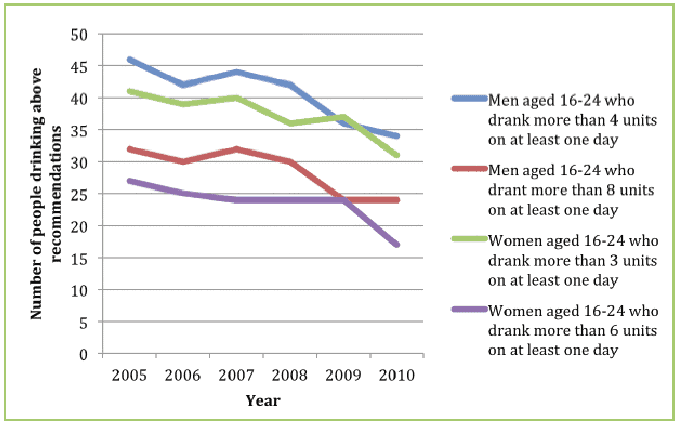
There is a downward trend in the maximum drunk on the heaviest drinking day. The proportions of both men and women who have exceeded twice the government’s recommended maximum consumption for a single day – the official definition of ‘binge drinking’ – has declined, the decline being most pronounced in the 16-24 age group.
Adults tend to drink more frequently as they get older. Over 1 in 5 men aged 65 and older drank almost every day, compared with just 3 per cent of men aged 16-24.
As is usually found, men and women in the managerial and professional categories tended to drink more and drink more frequently than those in routine and manual occupations. Normally, also, those with higher incomes tended to drink more and more frequently.
Interestingly, average weekly consumption was higher in adults living in rural areas than those in urban areas, the difference being driven by women.
Alcohol and obesity
A new report from the NHS National Obesity Observatory examines the relationship between obesity and alcohol consumption. The report suggests that there is no clear causal relationship between alcohol consumption and obesity, and the complex associations between the two are heavily influenced by a number of factors. These include patterns and levels of drinking, types of alcoholic drinks consumed, gender, body weight, diet, genes, physical activity levels and other lifestyle factors. However, there is a lack of clear evidence of the roles and interactions of all these factors, and the issue remains poorly understood. The report summarises what can be said about the subject:
- Many people are not aware of the calories contained in alcoholic drinks
- The effects of alcohol on body weight may be more pronounced in overweight and obese people
- Alcohol consumption can lead to an increase in food intake
- Heavy, but less frequent, drinkers seem to be at higher risk of obesity than moderate, frequent drinkers
- The relationships between obesity and alcohol consumption differ between men and women
- Excess body weight and alcohol consumption appear to act together to increase the risk of liver cirrhosis
- There is emerging evidence of a link between familial risk of alcohol dependency and obesity in women
Obesity and alcohol: an overview. National Obesity Observatory. February 2012
The report can be downloaded at: http://www.noo. org.uk/NOO_pub/ briefing_papers
One drink per day can increase breast cancer risk by 5%
A new review of research that looks at the relationship of alcohol consumption and breast cancer has been published in the journal Alcohol and Alcoholism. The analysis found that low level or moderate drinkers – one drink per day – had a 5% increased risk of breast cancer. Heavy alcohol consumption, defined as three or more drinks a day, was found to have a 40-50% increased risk of breast cancer. Overall, alcohol drinking accounts for roughly 5% of breast cancers in Northern Europe and North America and up to 10% in countries such as Italy and France, where drinking alcohol is common among women.
In Europe and the USA, breast cancer is the most common cancer in women. Several population studies have also shown that women have a high prevalence of light drinking. This represents a major health issue in terms of breast cancers and the western world. Alcohol consumption has been acknowledged as a risk factor for the development of cancer in various organs of the body for quite some years and an association between alcohol and breast cancer has been established since the 1980s. The review of research conducted by Helmut K. Seitz and Carlo La Vecchia et al, and published in Alcohol and Alcoholism, is entitled ‘Epidemiology and Pathophysiology of Alcohol and Breast Cancer: Update 2012’. The review analyses epidemiological data on the relationship of alcohol and breast cancer, looking at the possible mechanisms of alcohol-mediated breast cancer development.
Light alcohol consumption
When analysing the effects of light alcohol drinking, the authors reviewed research published before November 2011 via a literature search from MEDLINE, ISI Web of Science and EMBASE. In total, 3431 research papers were retrieved from the literature search. Of these, 113 papers reporting breast cancer risk estimates for light drinkers were included in the meta-analysis. The analysis included 44,552 cases in the reference category of nondrinkers and 77,539 cases in the light drinking category. 51% of studies were from North America, 38% from Europe, 6% from Asia and 10% from other regions. The meta-analysis of these studies reported a modest but significant association between light drinking and breast cancer. The estimate was based on the results of more than one hundred studies and found a small increase in risk, in the order of 5%, with the association between light drinking and breast cancer.
Dose-risk
The review carried out by Seitz and La Vecchia et al also found that each increased alcohol consumption increases the risk of breast cancer. This analysis showed a trend risk that was highly significant and there is consistent evidence for a positive dose-risk relation between alcohol and breast cancer.
Heavy Alcohol consumption
The largest collection of studies connecting the risk of breast cancer to alcohol was based on high level consumption of alcohol and cancer risk. The results indicated a 40-50% elevated risk of breast cancer in women consuming three or more drinks a day.
Hormone related mechanisms
Cancer of the female breast is slightly different to other body organ cancers as even small doses of alcohol can stimulate breast cancer development. As alcohol consumption might affect the risk of cancer through hormone-related mechanisms, the review published today in Alcohol and Alcoholism particularly looked at the association between alcohol consumption and the risk of breast cancer through hormone-related mechanisms such as estrogen receptor (ER) and progesterone receptor (PR) status. Seitz et al found that there was significant research to suggest that alcohol consumption increased the risk of all ER+ tumours by 27% and placed a 14% risk for all ER- breast cancers for the highest vs lowest level of alcohol drinking. Subsequent investigations by the team found further support for a stronger association between heavy alcohol consumption and ER+ breast cancers.
Studies investigating the mechanisms of ethanol-mediated breast cancer are rare and information is limited. However, a promotional effect of estrogens on breast tissue has been observed and since alcohol consumption causes elevated estrogen concentrations, it has been speculated that the carcinogenic effect of alcohol is mediated, in part, by estrogens. Seitz and La Vecchia et al discuss a number of study examples that provide further evidence on the role of estrogens in ethanol-mediated breast cancer and possible carcinogens for the breast. The observation that several studies support the hypothesis that alcohol is more strongly related to ER positive than ER negative breast tumours underlines the pathogenic role of estrogens in alcohol-mediated breast cancer.
“Epidemiology and Pathophysiology of Alcohol and Breast Cancer: Update”, Seitz, La Vecchia, et al, Alcohol and Alcoholism, doi: 10.1093/alcalc/ags011
Almost half of Londoners are worried about effects of alcohol on their health
Almost half of all Londoners are concerned about the long-term health effects caused by the amount of alcohol they drink, according to a survey of people living in the city.
The Regional Public Health Group, together with the Greater London Authority, has published a report detailing the results of a survey of 7,500 Londoners, which questioned them about alcohol consumption and the consequences.
The survey found almost half of Londoners (48%) are concerned about the long-term health issues linked to how much alcohol they drink. The survey highlights how important GPs are in providing initial support for people seeking help for alcohol problems. However, one fifth (19%) of respondents did not know where to turn for help, a figure which was significantly higher among people from lower socio-economic backgrounds and the 18-24-year-olds.
Dr Simon Tanner, Director of Public Health at NHS London, said: “We welcome this survey, which is the largest of its kind in London. It provides invaluable intelligence for local authorities as to how we can work together to tackle excessive drinking and its consequences, at a time when public health responsibilities move from PCTs to local government.”
Alcohol, with its links to violence, remains a public concern with almost three quarters (72%) of Londoners questioned feeling either quite or very concerned about alcohol-related crime and violence. The survey also found that many people feel local communities should have a larger role, with 51% of respondents believing that they could reduce local problems if involved in making decisions around managing alcohol issues.
Another finding of the survey was that more than half of the people questioned (52%) believe that employers should play a bigger role in providing access to advice on alcohol.
Will Tuckley, Chief Executive of London Borough of Bexley and Chair of the Alcohol Project Board, a workstream of the London Health Improvement Board, also welcomed the findings of the survey, saying: “There is no denying the health and societal consequences of alcohol misuse in local communities. However, what is missing from the debate is an understanding from the perspective of local residents and that is exactly what this survey has provided us with. As we move towards local authorities delivering key public health services it is critical that we understand the local issues and ensure that we use evidence to inform our local alcohol policies.”
The results of the survey follow the reopening of the Soho Alcohol Recovery Centre this weekend (February 24) which worked successfully over Christmas to provide an alternative to A & E for patients who have had too much to drink, while also freeing up A & E departments to deal with the most urgent cases. In December, staff at the centre treated around 180 patients who were taken there by response vehicles or ‘booze buses’. All patients have their blood pressure and sugar levels monitored while they sober up before they are discharged or family and friends are called to collect them. People are also given advice on drinking responsibly when they are discharged. The centre, which is run by London Ambulance Service and funded by NHS London, operated for a further five weekends from February 24.
Dr Tanner added: “We know the opening of the alcohol support centre will reduce pressure on A & E and beds within hospitals, but we know this is not a solution to the consequences of excessive drinking. We will be using these results to work with NHS services across the capital to find ways to raise awareness about the dangers of excessive drinking, as well as signpost patients to the correct place to get the help and advice they need.”
The London Summary Report is supported by individual London borough analysis, and can be accessed at:
http://www.lho.org.uk/ LHO_Topics/Health_Topics/ Lifestyle_and_behaviour/ londondrinkdebate.aspx
This Report follows the publication of Closing time: counting the cost of alcohol-attributable hospital admissions in London, published by the London Health Observatory, which provides estimates of the NHS inpatient resources used in treating patients whose alcohol use has contributed to their condition. This provides a basis for both pan-London comparison and local action. Both reports add to the evidence base in support of the London Health Improvement Board‘s (LHIB) priority to reduce the adverse impacts of alcohol on health.
The report can be accessed at: http://www.lho.org.uk/ viewResource.aspx?id=17713
Mayor welcomes new approach to alcohol-related crime in London
– but says more is needed
London will be the first city in England to trial a new scheme to tackle alcohol-related crime. After campaigning for further measures to be introduced, the Mayor of London, Boris Johnson, and his Deputy Mayor for Policing, Kit Malthouse, have been offered a new pilot scheme by the government for persistent alcohol offenders in the capital.
The ‘sobriety’ scheme will see criminals convicted of serious drink-related offences like assault or criminal damage given electronic tags that will be used to monitor alcohol in their blood. If the offenders continue to consume alcohol they will be arrested and brought before a judge who has the option of sending them back to prison.
This comes as a new Greater London Authority telephone survey of over a thousand Londoners found that over two thirds (69%) would welcome courts banning offenders from consuming alcohol if they were guilty of committing an alcohol-related offence, whilst 60% backed the right of courts to ban someone from consuming alcohol who has been given bail.
Across the UK, one fifth of all violent incidents take place in or around a pub or club. The majority (64%) of all violence occurs in the evening or at night and just under half occurs at the weekend (Friday 6pm until Sunday 6am).
The Mayor of London, Boris Johnson, said: “I am grateful to my colleagues in Whitehall for recognising that tackling crime is a top priority in this city and we must use every innovation at our disposal to keep on making London safer. This proposal is welcome but we still need the legislation passing to give the necessary powers in order to have a major impact.”
The Mayor is keen to continue working with the government on more comprehensive legislation to offer a wider scheme inspired by a programme in South Dakota led by Keith Humphreys, where 99.3% of offenders’ tests were negative and the prison population fell by 14%. Kit Malthouse, the Deputy Mayor for Crime and Policing said: “This pilot is great news for London and bad news for the persistent offenders who cause misery and mayhem with alcohol-fuelled violence. We hope this will now be the template for the wider reforms needed to fully implement the wider sobriety scheme we’re lobbying for which can successfully tackle wider issues like domestic violence and makes people pay for daily testing. The success of South Dakota proves that removing alcohol really reduces violent crime.
“In the meantime we hope this mini pilot will have a positive impact on 300 people this summer. Our alcohol survey proves the public want more done to tackle alcohol-related crime, so although criminals may protest, this may be the short sharp shock they need. Offenders will have to ask themselves if a drink is really worth a night in jail?”
In 2010/11 nearly half of all violent crime (almost 1 million crimes) was fuelled by alcohol and the police are fighting a constant and expensive battle against alcohol-related offences and antisocial behaviour. The London Ambulance Service attended 51,718 incidents in 2010/11 where alcohol was mentioned as involved – a 9% increase on the previous year.
The GLA survey also revealed that only 14 per cent of Londoners think that the costs for testing for alcohol sobriety should be met by the state – backing the lobbying of the Mayor’s Office for offenders to pay a small amount of money (around £1) towards daily breathalysing.
The total estimated cost of alcohol-related crime is £8bn to £13bn per year (Home Office). This estimate takes into account the costs in anticipation of crime, the direct physical and emotional costs to victims, the value of lost output, and the costs to the health service and Criminal Justice System.
Full topline results for the poll can be found at: http://www.london.gov.uk
Northern Ireland – 1 in 10 regular drinkers may have drinking problem
The latest Northern Ireland Drinking Survey, conducted on behalf of the Department of Health, Social Services and Public Safety, which examines the amount people drink, when, where and what they drink and who they drink with, finds that 1 in 10 of those who drink regularly may show some signs of alcohol dependence.
The key findings of the survey include:
Alcohol Consumption:
- More than 7 out of 10 (74%) adults drink alcohol
- A larger proportion of males (78%) than females (72%) drink alcohol
- Younger adults (18-29 years) are more likely to drink than older adults (60-75 years)
Frequency of Drinking:
- Around half (52%) of drinkers reported drinking alcohol at least once a week or more frequently (6% of respondents reported drinking on an almost daily basis)
- A greater proportion of male respondents (8%) compared to females (5%) reported drinking alcohol daily or on most days
Drinking Levels
Recommended daily drinking limits:
- Around 8 in 10 respondents (78%) reported having reached or exceeded the recommended daily limit for drinking on at least one occasion in the week prior to the survey
- 18% of male drinkers reached or exceeded the recommended daily limits on 3 or more days that week, compared to 16% of female drinkers
- The recommended daily limits are exceeded most often on a Saturday (53% of drinkers) and on a Friday (31% of drinkers)
Weekly guidelines for sensible drinking:
- More females (80%) compared to males (74%) stayed within the weekly guidelines for sensible drinking limits
Binge Drinking:
- 3 in 10 (30%) of those who drank in the week before the survey had engaged in at least one binge drinking session
- Males (35%) are more likely than females (25%) to binge drink
- Half (50%) of respondents in the youngest age group (18-29) who drank in the week prior to the survey had engaged in at least one binge drinking session compared to 13% of respondents in the oldest age group (60- 75)
Problem Drinking:
- CAGE question analysis (clinical interview questions) indicated that 1 in 10 (9%) of those who drank in the week prior to the survey are likely to have a problem with alcohol
- 6 in 10 (61%) of those who consumed alcohol in the week prior to the survey consider themselves to be light drinkers
- Just over one third (36%) consider themselves to be moderate drinkers and 3% consider themselves to be heavy drinkers
Adult drinking patterns in Northern Ireland 2011 The survey is available here: http://www.dhsspsni.gov.uk
Special Feature – Foetal Alcohol Syndrome
Damage to the unborn child is one of the main examples of the way in which alcohol can cause harm to people other than the drinkers themselves
Here, Stefan Lang, Medical Professionals Forum Administrator with the FASD Trust, describes the challenges of responding to the issue
There are two common misperceptions amongst a large proportion of the British population: firstly, that the long-term effects of drinking alcohol apply only to the individual in question. Secondly, that alcoholic consumption in moderation during pregnancy is an acceptable habit. These are not only sentiments held by the average person, but also by a number of the country’s medical professionals. The unfortunate result of this misinformation and laxity is an alarming prevalence of foetal alcohol spectrum disorders
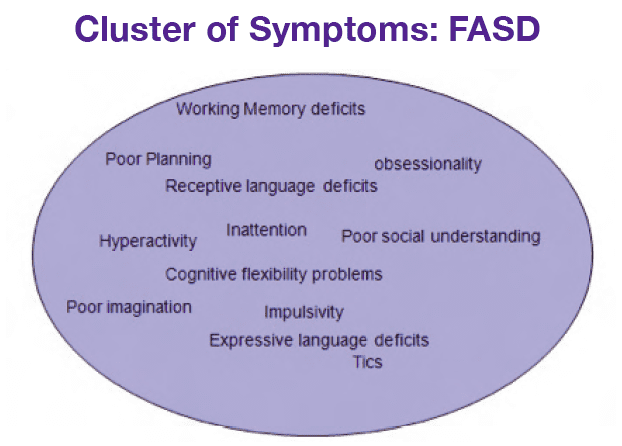
(FASD) in newborn babies across the country. FASD are caused by pre-natal exposure to alcohol. What is important to note is that even moderate amounts of alcohol ingestion by women during pregnancy are enough to leave a baby with FASD symptoms. These symptoms are a broad spectrum of structural anomalies and neurocognitive and behavioural disabilities, constituting Foetal Alcohol Syndrome (FAS) in its severest form. FAS is characterized by evidence of growth retardation, neuro-developmental abnormalities, and a characteristic pattern of facial anomalies. (See Fig. 1 below)
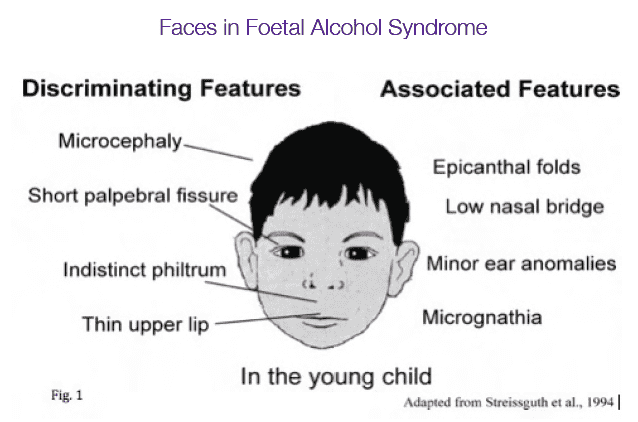
In a study at the University of California, San Diego, Haruna Sawada Feldman found that “Higher prenatal alcohol exposure in every alcohol consumption pattern was significantly linked to an increased risk of the baby being born with reduced birth weight or length, having a smooth philtrum, thin vermillion border or microcephaly”. Meanwhile, a study in Denmark concluded that even minimal drinking during pregnancy doubles the risk of a miscarriage or causing damage to an unborn child. Dr. Anne-Marie Nybo Andersen said, “If our risk estimates are correct, it’s best not to drink at all” during pregnancy.
That said some experts believe as many as one in three-hundred newborn children in the UK could be suffering from FASD. Accurate statistics are, however, difficult to come by. Although there was a 41% increase in alcohol-related hospital admissions for women aged 15- 44 between 2003 and 2008, diagnosed cases of FASD did not rise. This, according to Dr. Shirin Howell, “suggests that FASD is materially under-reported in the UK.” In order to change this worrying state of affairs, greater awareness for tackling FASD, from prevention to diagnosis to management, is essential. To achieve this, a lot of lost time needs to be made up.
Challenges of Tackling FASD in the UK
The idea that it is “bad to drink when you’re pregnant” is commonly accepted in the UK. However, it is not ingrained in our culture as it is in the US, for example. There, FASD was clinically diagnosed in 1973, and from as early as 1980 women were actively encouraged by GPs and paediatricians to refrain from drinking throughout the duration of their pregnancies, from conception to birth. One need only look at the abundant academic literature on FASD in America in relation to the UK to see the seriousness with which it’s been taken across the Atlantic.
Because FASD have been so poorly publicised in the UK, there is still a fairly relaxed attitude towards pregnant drinking. Indeed, in 2007 The National Institute for Health and Clinical Excellence published guidelines stating that it was safe for pregnant women to drink 1.5 units of alcohol a day without harming their unborn child. Until recently, many women were even encouraged to drink the odd glass of wine by doctors as a means of preventing early labour. Such archaic methods and advice show how far the UK has to come. It could be argued that this arrogance is a result of Britain’s more epidemic drinking “culture”. For some people, it seems, drinking alcohol is such a stable part of their lifestyle that giving-up during pregnancy is too much to ask. That is where community, and national, support is necessary. Prevention is achievable with the complicit help of schools, medical clinics and public organisations. Otherwise, a child is burdened by an incurable condition for life.
And that is not the end of the difficulties. By diagnosing FASD at an early stage in a child’s life, management structures can be put in place to aid their development. Unfortunately, many doctors in the UK find it difficult to diagnose FASD. With such a wide array of symptoms, FASD children are often defined as autistic or as suffering from ADHD or dyspraxia. Whilst they may have some of the symptoms associated with these conditions, their cases are often far more complex and require more considered attention. If we fail to raise awareness amongst the public and medical professionals then misdiagnoses will persist, to the detriment of children and carers alike.
The FASD Trust
Raising awareness is the goal of the FASD Trust, an Oxfordshire-based charity started by Julia and Simon Brown. By taking a dual-approach, which involves targeting not only community leaders, but medical professionals, the Trust seeks to end the casual approach to pre-natal drinking in the UK. One of its key strategies in achieving this lofty goal is through the creation of a Medical Professionals Forum. The Forum’s membership consists of doctors in the fields of paediatrics, CAMHS, psychiatry and psychology and aims to provide a setting for sharing sensitive casework and research on FASD. By using the existing networks of medical professionals, the Trust hopes to spread its message further afield. The Forum provides an education for medics so that they are better-able to diagnose FASD as early as possible and simultaneously advise parents and carers on the management of children with FASD. This is a far more effective method than simply delivering leaflets to schools and community institutions, which alone will not create the national awareness of FASD that is required.
Of course, the FASD Trust takes an active role in the community as well. By running a network of regional support groups for FASD sufferers and their carers, the Trust provides guidance for hundreds of people in need of respite. Whilst early diagnosis is crucial, the management of FASD is even more so, for it is a lifelong responsibility. Medical help can only go so far; it is the carers that shoulder the greatest burden in looking after people with FASD, from childhood to adulthood. This can understandably be overwhelming for many people and is where the Trust works to offer support, based on both medical advice and personal experience. Furthermore, through establishing partnerships with local schools the Trust serves another double purpose. First, it encourages teachers to emphasise to their students the importance of avoiding alcohol during pregnancy, thus minimising the risk of ignorance amongst young parents. Second, it gives teachers direction in dealing with pupils suffering from FASD so that classes are not disrupted, and so that those with FASD receive the best possible education within their limitations.
Preventable
Perhaps the most shocking fact about FASD is that it is entirely preventable. It is only caused by the baby ingesting alcohol when in the womb; a choice taken on its behalf by the mother. To think that thousands of people in the UK, and their carers, are faced with life-long repercussions because of a person’s selfishness or ignorance is saddening. Encouragingly, the FASD Trust and its forum are proving that medical attitudes towards FASD in the UK are changing. Only through collaboration between the medical world and the community at large can we hope to reverse the worrying trends of FASD case-prevalence in this country.
In addition, by offering expert advice and dedicated support groups, the Trust helps improve the lives of those affected by FASD. Despite their disabilities, people with FASD are capable of great empathy and affection, whilst having a positive attitude towards their surrounding environment. It is essential to nurture this positivity.
We have created the FASD issue. Only through our concerted effort and support can we alleviate the strains placed on the innocent victims of our alcohol-fuelled society.
Podcast
Our monthly podcast features interviews with experts from across the sector.
Gambling industry harms and parallels with the alcohol world
Will Prochaska –
Coalition to End Gambling Ads

